Aortic stenosis is a common heart valve disease that occurs when the aortic valve narrows, leading to restricted blood flow from the heart to the rest of the body. It is most commonly caused by age-related degeneration or a congenital heart defect.
In severe cases, it can significantly impair the heart’s ability to pump blood effectively.
Understanding Aortic Valve Replacement
Aortic valve replacement (AVR) is a surgical procedure that involves replacing the damaged aortic valve with an artificial valve.
It is the standard treatment for patients with severe aortic stenosis who experience symptoms or have evidence of significant heart damage. The goal of AVR is to restore normal blood flow through the aorta and improve the patient’s quality of life.
Indications for Aortic Valve Replacement
The timing of AVR is crucial in determining its effectiveness. The decision to undergo valve replacement is based on a combination of factors, including symptoms, valve anatomy, and the presence of other comorbidities. Here are the indications for AVR:.
- Symptomatic Patients: Individuals with severe aortic stenosis who experience symptoms such as chest pain, shortness of breath, fatigue, or fainting.
- Left Ventricular Dysfunction: Patients with evidence of reduced left ventricular function due to aortic stenosis.
- Abnormal Exercise Test: Abnormal stress test results indicating impaired cardiac function during exercise.
- Severely Calcified Aortic Valve: Aortic valve stenosis with extensive calcification, leading to valve obstruction.
- Another Cardiac Surgery: Patients undergoing other cardiac surgeries, such as coronary artery bypass grafting, who also have significant aortic stenosis.
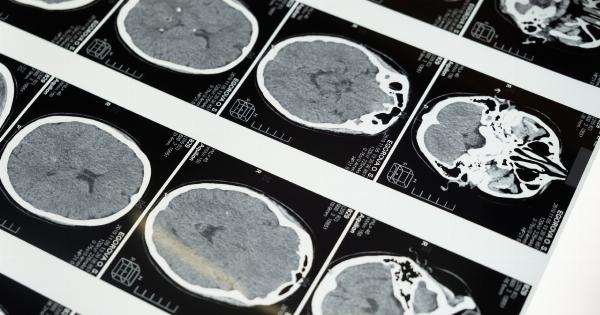
Evaluation and Risk Stratification
Before recommending AVR, a thorough evaluation is necessary to assess the patient’s overall health and determine the risk associated with the procedure. Risk stratification is crucial as it assists in selecting the optimal timing for surgery.
Several factors are considered, including:.
- Age: Advanced age alone is not a contraindication for surgery. However, it may increase the risk of complications.
- Symptoms: The severity and impact of symptoms on the patient’s quality of life are important considerations.
- Left Ventricular Function: Impaired left ventricular function indicates advanced disease and may necessitate earlier surgery.
- Exercise Tolerance: Patients with reduced exercise tolerance or abnormal exercise test results may benefit from early intervention.
- Comorbidities: The presence of other medical conditions, such as kidney disease or lung disease, may influence the risk-benefit analysis.
Timing Considerations for Aortic Valve Replacement
The optimal timing for AVR depends on several factors, including symptoms, disease progression, and the risk associated with surgery. The decision should be a shared decision-making process involving the patient, their family, and the healthcare team.
Here are the three timing categories:.
Early Surgery
Early surgery is recommended for patients with severe symptomatic aortic stenosis or evidence of left ventricular dysfunction. Symptoms may include angina (chest pain), dyspnea (shortness of breath), syncope (fainting), or heart failure symptoms.
Early surgery aims to prevent irreversible heart damage and improve overall prognosis.
Watchful Waiting
In patients with asymptomatic severe aortic stenosis, a conservative approach of active surveillance, also known as watchful waiting, may be adopted.
This involves regular monitoring of symptoms and periodic cardiac evaluations to detect any changes in the patient’s condition. Watchful waiting is typically recommended to individuals with low surgical risk and a lack of symptoms.
Prophylactic Surgery
Prophylactic surgery refers to performing AVR in asymptomatic patients who have high-risk characteristics. These high-risk features may include rapid disease progression, abnormally elevated stress test results, or abnormal findings on imaging studies.
Prophylactic surgery aims to minimize the risk of sudden deterioration and adverse cardiac events.
Advancements in Aortic Valve Replacement
Over the years, there have been significant advancements in AVR techniques, leading to improved patient outcomes and reduced surgical risks. Here are some notable advancements:.
- Transcatheter Aortic Valve Replacement (TAVR): TAVR is a minimally invasive procedure that involves delivering a new valve through a catheter, typically inserted with a small incision in the groin. It is an alternative option for patients who are considered high-risk or inoperable for traditional open-heart surgery.
- Minimally Invasive AVR: Traditional AVR typically requires a sternotomy (division of the breastbone). Minimally invasive AVR uses smaller incisions, resulting in shorter hospital stays, faster recovery, and less pain for patients.
- Robotic-Assisted AVR: Robotic-assisted AVR involves the use of robotic arms controlled by a surgeon to perform the valve replacement surgery. It offers increased precision and flexibility, leading to enhanced outcomes.
- Sutureless Valve Replacement: Sutureless AVR uses a self-expanding valve that eliminates the need for traditional sutures. It allows for faster implantation and reduces surgical times.
Conclusion
Aortic valve replacement is a critical treatment option for patients with severe aortic stenosis. Timing is essential in determining the optimal approach for each individual, considering symptoms, disease progression, and surgical risk.
With advancements in surgical techniques, patients now have access to various options, including minimally invasive procedures and transcatheter valve replacements. A thorough evaluation and shared decision-making process between the patient and healthcare team are crucial in achieving the best outcomes for those with aortic stenosis.