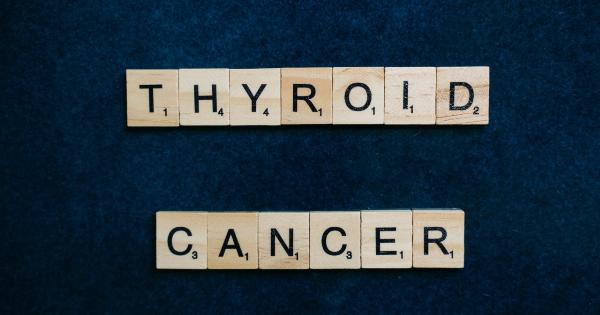
Thyroid cancer has become one of the fastest-growing cancer types in recent years. According to the American Cancer Society, the number of thyroid cancer cases has been steadily increasing over the past few decades.
However, the rise in diagnoses does not necessarily mean that there has been a surge in actual cancer cases. Instead, the increase can be attributed to improved diagnostic methods and increased awareness, leading to the detection of smaller, previously undetectable tumors.
Dilemma of Thyroid Nodules
One of the main challenges in thyroid cancer diagnosis is the presence of thyroid nodules. These nodules are small lumps that can develop in the thyroid gland and are incredibly common.
In fact, studies have shown that nearly 50% of people over the age of 50 have thyroid nodules. However, the majority of these nodules are benign and do not pose a threat to health.
Traditionally, when a thyroid nodule is discovered, the next course of action would be to perform a surgical procedure, such as a thyroidectomy, to determine if the nodule is cancerous or not.
This approach often leads to unnecessary surgeries, as the majority of nodules turn out to be benign. Not only does this unnecessarily expose patients to the risks associated with surgery, but it also adds to the financial burden of the healthcare system.
A Game-Changing Diagnostic Test
Fortunately, there has been significant progress in the field of thyroid cancer diagnostics.
A recent breakthrough in diagnostic testing has revolutionized the way thyroid nodules are evaluated, minimizing unnecessary surgeries and improving patient outcomes. This innovative test is known as the Thyroid FNA Genomic Classifier.
The Thyroid FNA Genomic Classifier is a molecular test that examines the genetic makeup of thyroid cells obtained through a fine-needle aspiration (FNA) biopsy.
By analyzing the genetic material, the test can accurately determine the likelihood of a thyroid nodule being cancerous or benign. This allows for a more targeted and precise approach, reducing the need for unnecessary surgeries.
The Power of Precision Medicine
The development of the Thyroid FNA Genomic Classifier highlights the power of precision medicine in improving healthcare outcomes.
Precision medicine, also known as personalized medicine, aims to tailor medical treatment to the individual characteristics of each patient, including their genetic makeup.
Prior to the availability of this diagnostic test, many patients with thyroid nodules underwent surgery, which may have been unnecessary.
With the introduction of the Thyroid FNA Genomic Classifier, physicians can now make more informed decisions about whether surgery is truly necessary or if other monitoring or treatment options should be pursued.
Precision medicine allows for a more targeted and individualized approach to healthcare, reducing unnecessary interventions and improving patient well-being.
By integrating genetic information into medical decision-making, precision medicine is transforming the way we diagnose and treat diseases, including thyroid cancer.
The Benefits of the Thyroid FNA Genomic Classifier
The Thyroid FNA Genomic Classifier offers several significant benefits over traditional diagnostic methods, ultimately leading to a reduction in unnecessary surgeries:.
1. Increased Accuracy
Traditional diagnostic methods, such as ultrasound and fine-needle aspiration, can yield inconclusive results in some cases. This uncertainty often leads to surgical intervention to obtain a definitive diagnosis.
The Thyroid FNA Genomic Classifier, however, provides a more accurate assessment of the likelihood of malignancy, reducing the need for surgery in cases where the likelihood of cancer is low.
2. Improved Patient Outcomes
By avoiding unnecessary surgeries, patients experience less physical and emotional trauma associated with invasive procedures.
Additionally, the financial burden of surgery is alleviated, as healthcare resources can be directed towards those who truly require surgical intervention.
3. Cost-Effectiveness
In addition to the improved patient outcomes, the Thyroid FNA Genomic Classifier is a cost-effective solution. It eliminates the need for unnecessary surgeries, which are not only expensive but also require extensive postoperative care.
By reducing the number of surgeries, healthcare costs can be significantly reduced, benefiting both patients and the healthcare system as a whole.
4. Preservation of Thyroid Function
Surgical removal of the thyroid gland, known as a thyroidectomy, can result in the loss of thyroid function and the need for lifelong hormone replacement therapy.
By accurately identifying benign nodules, the Thyroid FNA Genomic Classifier helps preserve the thyroid gland and its normal function, avoiding potential complications associated with surgery.
5. Efficient Resource Allocation
By reducing the number of unnecessary surgeries, the Thyroid FNA Genomic Classifier allows healthcare resources to be allocated more efficiently.
Surgical and hospital resources can be directed towards patients who truly require invasive treatment, ensuring that those in need receive timely and appropriate care.
Conclusion
The development and adoption of the Thyroid FNA Genomic Classifier have brought about a significant breakthrough in the diagnosis of thyroid cancer.
This molecular test has revolutionized the field, minimizing unnecessary surgeries and improving patient outcomes. By accurately identifying malignant and benign thyroid nodules, physicians can provide more targeted and personalized care, sparing patients from unnecessary procedures and the associated physical, emotional, and financial burden.
As precision medicine continues to advance, we can expect more innovative diagnostic tests like the Thyroid FNA Genomic Classifier to emerge, improving the accuracy of disease diagnosis and revolutionizing the way we approach healthcare.