Sleep apnea is a common sleep disorder characterized by repetitive pauses in breathing during sleep. These pauses, known as apneas, can last for a few seconds to minutes and occur multiple times throughout the night.
Sleep apnea can lead to fragmented sleep and reduced oxygen supply to the brain and other organs.
Recent studies have suggested a potential link between sleep apnea and Alzheimer’s disease, a degenerative brain disorder that affects memory, thinking, and behavior.
While the exact nature of the relationship between the two conditions is still being investigated, several mechanisms have been proposed to explain the association.
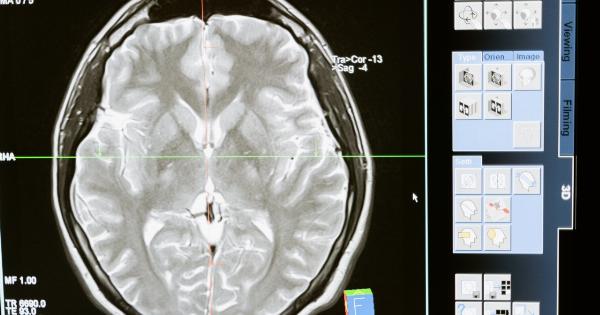
The Impact of Sleep Apnea on Brain Health
During an apnea event, the brain is deprived of oxygen, leading to a drop in blood oxygen levels.
This can trigger a cascade of physiological responses, including oxidative stress, inflammation, and changes in the production and clearance of beta-amyloid and tau proteins – the hallmarks of Alzheimer’s disease.
Oxidative stress occurs when there is an imbalance between the production of damaging free radicals and the body’s ability to neutralize them.
The brain is particularly vulnerable to oxidative stress due to its high oxygen consumption and abundance of polyunsaturated fatty acids. Chronic repetitive episodes of oxygen deprivation and reoxygenation associated with sleep apnea can exacerbate oxidative stress and contribute to the accumulation of reactive oxygen species, leading to cellular damage.
Inflammation is another key pathophysiological process implicated in both sleep apnea and Alzheimer’s disease.
Sleep apnea has been shown to increase the production of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These inflammatory markers may promote neuroinflammation and contribute to neuronal injury and synaptic dysfunction.
Beta-amyloid and tau proteins are known to play a central role in the development and progression of Alzheimer’s disease.
In individuals with sleep apnea, the clearance of beta-amyloid is impaired, leading to an accumulation of the protein in the brain. This may trigger a series of events that ultimately contribute to the formation of amyloid plaques and the neurofibrillary tangles characteristic of Alzheimer’s disease.
The Impact of Sleep Disruption on Cognitive Function
Aside from the physiological changes associated with sleep apnea, the fragmented sleep patterns it causes can have a direct impact on cognitive function.
Sleep is crucial for memory consolidation and neuronal repair, and disruptions in sleep architecture can impair these processes.
Individuals with sleep apnea often experience excessive daytime sleepiness and cognitive impairment.
These cognitive deficits may manifest as difficulties with attention, concentration, memory, and executive function – all of which are also common symptoms in Alzheimer’s disease. There is evidence to suggest a bidirectional relationship between sleep disturbances and cognitive decline, whereby sleep disruption exacerbates cognitive impairment, and cognitive decline further disrupts sleep.
Epidemiological Evidence
Several population-based studies have provided insights into the potential link between sleep apnea and Alzheimer’s disease.
These studies have consistently reported an increased risk of cognitive decline and dementia in individuals with sleep-disordered breathing, including sleep apnea.
A longitudinal study conducted by Yaffe et al.
followed older women for nearly five years and found that those with sleep-disordered breathing at baseline had a significantly higher risk of developing mild cognitive impairment or dementia during the follow-up period compared to those without the disorder. Another study by Osorio et al. demonstrated that individuals with sleep apnea showed significantly higher levels of beta-amyloid in the brain, further supporting the connection with Alzheimer’s disease.
Furthermore, a systematic review and meta-analysis of observational studies concluded that individuals with sleep apnea had a 26% higher risk of developing cognitive impairment or dementia compared to those without sleep-disordered breathing.
Treatment Implications
The potential link between sleep apnea and Alzheimer’s disease highlights the importance of effective diagnosis and treatment of sleep-disordered breathing.
Continuous positive airway pressure (CPAP) therapy is the gold standard treatment for sleep apnea and involves wearing a mask over the nose or mouth during sleep, which delivers a continuous stream of air to keep the airways open.
Several studies have investigated the impact of CPAP therapy on cognitive function in individuals with sleep apnea. While some studies have shown cognitive improvements following treatment, the results have been mixed.
Further research is needed to determine the effects of CPAP therapy on cognitive decline and the prevention of Alzheimer’s disease.
Additionally, lifestyle modifications such as weight loss, regular exercise, and sleep hygiene practices can help alleviate sleep apnea symptoms and improve overall sleep quality.
These lifestyle interventions may also have a positive impact on cognitive health and reduce the risk of Alzheimer’s disease.
Conclusion
Sleep apnea is increasingly recognized as a potential risk factor for Alzheimer’s disease. The underlying mechanisms linking the two conditions include oxidative stress, inflammation, impaired protein clearance, and sleep disruption.
Epidemiological studies have consistently shown an association between sleep apnea and cognitive decline or dementia.
Further research is needed to elucidate the complex relationship between sleep apnea and Alzheimer’s disease and to evaluate the potential benefits of treating sleep-disordered breathing in preventing or delaying cognitive decline.
Early identification and effective management of sleep apnea may not only improve sleep quality and quality of life but also have important implications for brain health and the prevention of Alzheimer’s disease.