Tuberculosis (TB) is a persistent and deadly infectious disease that primarily affects the lungs. It is caused by the bacteria Mycobacterium tuberculosis and is transmitted through the air when an infected individual coughs or sneezes.
Despite being preventable and curable, TB remains a significant global health concern, especially in low and middle-income countries.
The Global Burden of Tuberculosis
TB is one of the top 10 causes of death worldwide and the leading cause of death from a single infectious agent.
According to the World Health Organization (WHO), an estimated 10 million people fell ill with TB, and 1.4 million died from the disease in 2019 alone. TB is a major public health issue, particularly in resource-limited settings, where poverty, crowded living conditions, and limited access to healthcare contribute to its prevalence.
Treatment Disparities
Addressing treatment disparities is crucial in the global fight against TB.
Despite the availability of effective treatments, many individuals with TB are unable to access or complete their treatment, leading to poor health outcomes and increased transmission of the disease. Several factors contribute to these treatment disparities, including:.
Limited Access to Healthcare
One of the main barriers to TB treatment is limited access to healthcare services, especially in remote and marginalized communities.
Inadequate infrastructure, health worker shortages, and financial barriers prevent individuals from seeking timely diagnosis and treatment. Efforts to expand healthcare infrastructure and improve access to diagnostic and treatment facilities are essential in addressing this disparity.
Stigma and Discrimination
TB is often associated with social stigma and discrimination, which can prevent individuals from seeking diagnosis and treatment.
Fear of being isolated, judged, or ostracized by their communities leads many people to hide their symptoms or delay seeking care. Promoting awareness, education, and community engagement initiatives can help reduce the stigma associated with TB and encourage individuals to seek the treatment they need.
Diagnostic Challenges
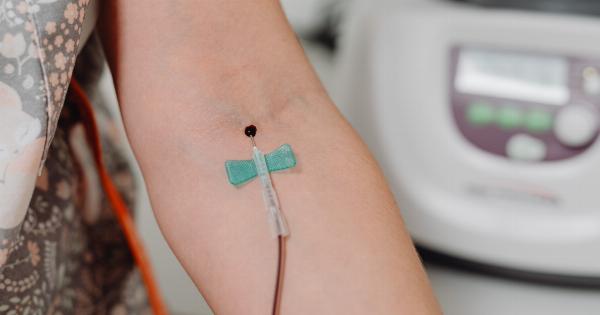
Many individuals with TB go undiagnosed or experience delays in diagnosis due to limitations in diagnostic tools and protocols. Traditional methods, such as sputum smear microscopy, have lower sensitivity and may not detect all cases of TB.
Implementing newer, more accurate diagnostic techniques, such as GeneXpert MTB/RIF or Xpert Ultra, can improve early detection and prompt initiation of treatment.
Drug Resistance
The emergence of drug-resistant strains of TB, particularly multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), poses a significant challenge to effective treatment.
These strains do not respond to the standard first-line drugs used to treat TB, requiring longer, more costly, and often more toxic treatment regimens. Ensuring access to appropriate diagnostic tests and effective second-line drugs is crucial in addressing the treatment disparities associated with drug-resistant TB.
Adherence and Treatment Completion
Adherence to TB treatment regimens is essential for successful outcomes. However, many individuals face difficulties in completing their treatment due to various factors.
Poverty, transportation costs, medication side effects, and the lack of support systems can lead to treatment interruptions or non-adherence. Implementing patient-centered approaches, including directly observed therapy (DOT), community-based support, and financial incentives, can help improve treatment adherence and completion rates.
Integration of TB Services
Integrating TB services with other healthcare programs, such as HIV/AIDS, maternal and child health, and primary care, can improve access to TB diagnosis and treatment.
Many individuals with TB also suffer from co-morbidities, and integrating services can ensure comprehensive care and address treatment disparities associated with concurrent health conditions.
Health Education and Awareness
Health education and awareness campaigns play a critical role in addressing TB treatment disparities.
Empowering communities with knowledge about TB, its symptoms, transmission, and the importance of seeking timely diagnosis and treatment can help overcome misconceptions and encourage early healthcare-seeking behaviors.
Cross-Border Collaboration
TB does not recognize international borders, and addressing treatment disparities requires cross-border collaboration.
Sharing resources, expertise, and best practices among countries can improve the availability and quality of TB diagnosis and treatment services, particularly in border regions where mobility and migration contribute to the spread of the disease.
Investment in Research and Innovation
Continued investment in research and innovation is crucial for improving TB treatment and reducing disparities. Developing new diagnostic tools, shorter and more effective treatment regimens, and vaccines are essential in the global fight against TB.
Governments, research institutions, and pharmaceutical companies should collaborate to ensure the availability and affordability of new technologies to all individuals in need.
Conclusion
Addressing TB treatment disparities is vital to eradicate the disease and reduce its burden worldwide.
Improving access to healthcare, reducing stigma, enhancing diagnostic capabilities, tackling drug resistance, promoting adherence, integrating services, focusing on health education, fostering cross-border collaboration, and investing in research are essential components of a comprehensive strategy to achieve equitable and effective TB treatment.