Endoscopy is a medical procedure that allows doctors to visualize and examine the internal organs and structures of the body.
Over the years, advancements in endoscopic imaging and technology have revolutionized the field of medicine, enabling earlier and more accurate diagnoses, as well as minimally invasive treatments. In this article, we will explore some of the notable advancements in endoscopic imaging and technology.
1. High-definition Endoscopy
One of the significant advancements in endoscopic imaging is the introduction of high-definition (HD) technology. HD endoscopes provide enhanced image quality, allowing doctors to see more detailed views of the internal organs.
This improvement in image resolution aids in better detecting abnormalities, smaller lesions, and precise targeting during procedures. HD endoscopy has become the standard in many gastrointestinal procedures, such as colonoscopy and gastroscopy.
2. Narrow Band Imaging (NBI)
Narrow Band Imaging is a specialized endoscopic imaging technology that enhances the visualization of the mucosal surface of organs. It works by using specific light wavelengths to highlight blood vessels and surface patterns more effectively.
NBI enables better differentiation between healthy and abnormal tissue, especially in the gastrointestinal tract. This technology has significantly improved the detection and characterization of early-stage cancers and precancerous lesions.
3. Confocal Laser Endomicroscopy (CLE)
Confocal Laser Endomicroscopy is a real-time imaging technique that allows for microscopic visualization of tissue structures during endoscopy. It uses laser light to generate high-resolution images deep within the tissues.
CLE provides real-time visualization of cellular and subcellular structures, aiding in the identification of abnormalities at a microscopic level. This technology has proven valuable in diagnosing conditions like Barrett’s esophagus and inflammatory bowel disease.
4. Endoscopic Ultrasound (EUS)
Endoscopic Ultrasound combines traditional endoscopy with ultrasound imaging technology. It allows for detailed imaging of the digestive tract wall layers as well as surrounding structures such as lymph nodes and blood vessels.
EUS plays a critical role in diagnosing and staging gastrointestinal cancers, as well as evaluating and guiding therapeutic interventions like needle biopsies and drainage procedures. The addition of Doppler imaging to EUS further enhances its diagnostic capabilities.
5. Virtual Chromoendoscopy
Virtual Chromoendoscopy is a non-invasive technique that mimics the effect of traditional chromoendoscopy without the need for dyes or stains.
This technology uses advanced image processing algorithms to highlight specific tissue features and patterns, aiding in the detection and characterization of abnormalities. Virtual Chromoendoscopy has been particularly effective in improving the detection of small polyps and flat lesions in the colon and esophagus.
6. Capsule Endoscopy
Capsule Endoscopy involves the ingestion of a small, wireless capsule that captures images of the digestive tract as it passes through.
The images are transmitted to a data recorder worn by the patient, which can be later analyzed by a healthcare professional. This technology is mainly used for visualizing the small intestine, an area that is challenging to reach with traditional endoscopy.
Capsule endoscopy has revolutionized the diagnosis and management of small bowel diseases such as Crohn’s disease and obscure gastrointestinal bleeding.
7. Robotic Assisted Endoscopy
Robotic Assisted Endoscopy combines the precision and maneuverability of robotic systems with endoscopic procedures. Robotic arms equipped with surgical instruments are controlled by the surgeon to perform complex endoscopic maneuvers.
This technology allows for increased dexterity and improved accuracy during procedures, particularly in difficult-to-reach anatomical locations. Robotic Assisted Endoscopy has been utilized in various applications, including surgery for gastrointestinal cancers and advanced endoscopic resections.
8. Fluorescence Imaging
Fluorescence Imaging involves the use of fluorescent agents injected into the body to enhance visualization during endoscopy. When exposed to specific light wavelengths, these agents emit fluorescence, highlighting areas of interest.
Fluorescence imaging allows for improved visualization of blood vessels, lymphatic systems, and specific molecular targets. It has found applications in different specialties, such as urology, gastroenterology, and pulmonology.
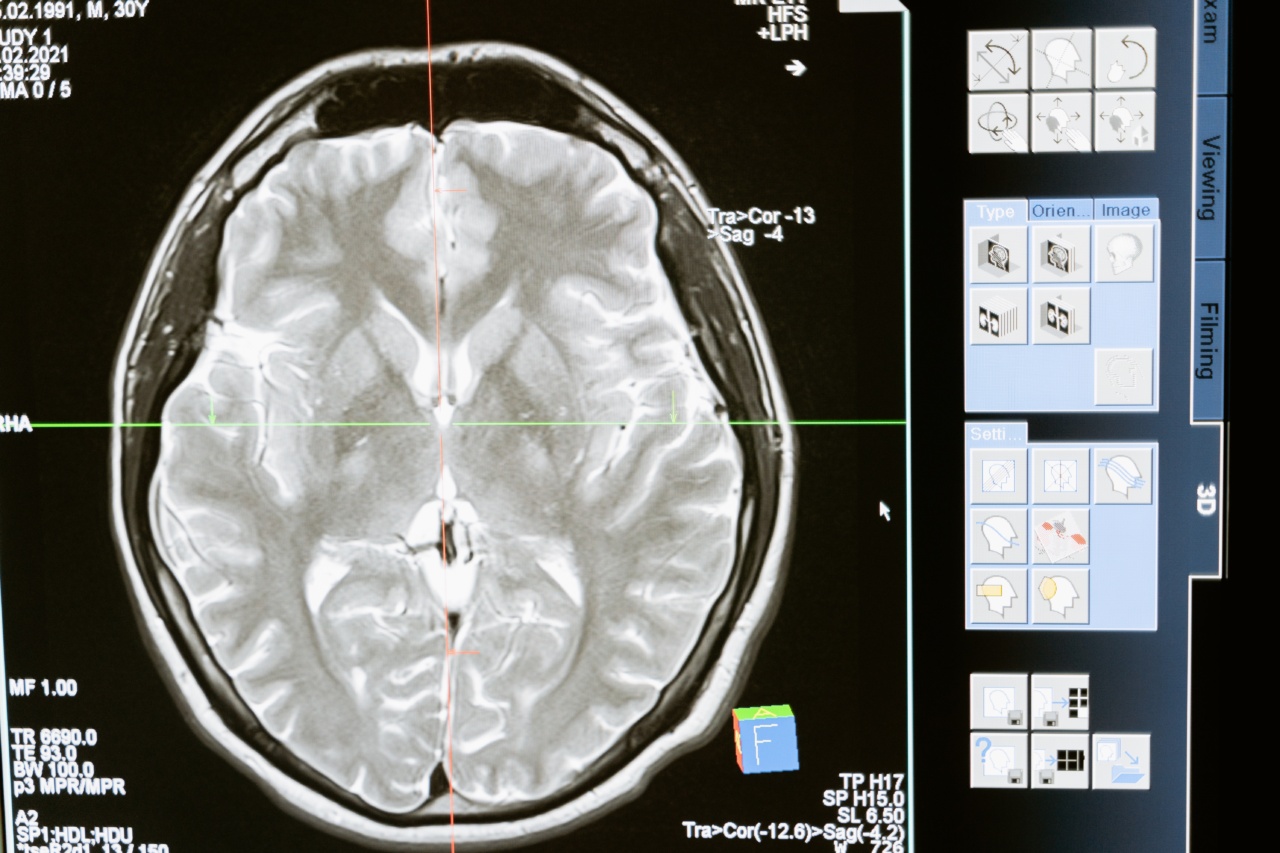
9. 3D Endoscopy
Three-dimensional (3D) Endoscopy provides a more immersive and realistic visualization of the internal organs compared to traditional 2D imaging.
It uses stereoscopic imaging technology to recreate depth perception, enhancing the surgeon’s ability to perceive spatial relationships during procedures. This advancement improves the accuracy of interventions, especially in complex anatomical regions. 3D endoscopy has been employed in various specialties, including neuroendoscopy, urology, and laparoscopy.
10. Artificial Intelligence (AI)
Artificial Intelligence is playing an increasingly prominent role in endoscopic imaging and technology. AI algorithms can analyze large volumes of endoscopic images and videos to aid in real-time decision-making, lesion detection, and risk assessment.
AI tools have demonstrated promising results in the detection of colon polyps, esophageal lesions, and early-stage gastrointestinal cancers. The integration of AI into endoscopy systems holds great potential for improving diagnostic accuracy and efficiency.