Diabetes is a complex metabolic disorder that affects various systems in the body, including bone health.
While diabetes is primarily known for its impact on blood sugar levels and its association with cardiovascular complications, it also significantly affects bone metabolism and increases the risk of bone-related complications. People with diabetes have a higher likelihood of developing osteoporosis, decreased bone density, fractures, and other bone-related issues.
Understanding the connection between diabetes and bone health is crucial for effective prevention and management strategies. This article discusses the complications associated with bone health in diabetes and explores preventive measures and treatments.
1. Osteoporosis and Decreased Bone Density
Osteoporosis is a condition characterized by low bone mass and structural deterioration of bone tissue, leading to increased fragility and susceptibility to fractures.
Studies have found that people with diabetes have a higher risk of developing osteoporosis and decreased bone density compared to the general population. The exact mechanisms underlying this connection are not fully understood, but several factors are believed to contribute to the increased risk:.
a) Insulin deficiency or resistance: Insulin plays a vital role in bone metabolism by promoting the production of osteoblasts, the cells responsible for bone formation.
In diabetes, insulin deficiency or resistance may impair the osteoblastic activity, leading to reduced bone formation.
b) Chronic inflammation: Diabetes is associated with chronic low-grade inflammation, which can adversely affect bone health. Inflammatory cytokines produced in diabetes disrupt the balance between bone formation and resorption, favoring bone loss.
c) Vitamin D deficiency: Vitamin D is essential for maintaining bone health as it helps in the absorption of calcium and promotes bone mineralization.
Deficiency of vitamin D is prevalent among individuals with diabetes, especially those with poor glycemic control, increasing the risk of osteoporosis.
2. Increased Risk of Fractures
Individuals with diabetes have a higher propensity for fractures, even in the absence of osteoporosis. Fractures occur more frequently in diabetes due to various factors:.
a) Impaired bone quality: Diabetes affects bone quality by reducing collagen cross-linking, impairing bone remodeling, and altering the composition of bone matrix.
These changes weaken the structural integrity of the bones, making them more susceptible to fractures.
b) Neuropathy: Diabetic neuropathy, a common complication of diabetes, affects the nerves responsible for perceiving pain and proprioception.
As a result, individuals with diabetic neuropathy may experience a loss of sensation in their extremities, making them more prone to falls and fractures.
c) Medications: Certain medications used to manage diabetes, such as thiazolidinediones, have been linked to an increased risk of fractures. These medications may negatively affect bone health by reducing bone density and impairing bone quality.
3. Diabetic Foot Ulcers and Amputation
Diabetic foot ulcers are a severe complication of diabetes that can lead to infection, gangrene, and ultimately, amputation. While foot ulcers primarily result from poor blood circulation and peripheral neuropathy, bone health also plays a crucial role.
Chronic hyperglycemia impairs bone healing and remodeling, delaying the closure of ulcers and increasing the risk of infections. In severe cases, the infection can progress to the bone, leading to osteomyelitis and necessitating amputation to prevent the spread of infection.
4. Hypoglycemia and Bone Health
Hypoglycemia, a common side effect of insulin or certain diabetes medications, has also been associated with bone health complications.
Prolonged and recurrent episodes of hypoglycemia can negatively impact bone mineral density and increase the risk of fractures. Hypoglycemia affects bone health by disrupting the balance between bone formation and resorption, leading to decreased bone mass.
5. Impaired Kidney Function
Diabetes is a leading cause of kidney disease, also known as diabetic nephropathy. Impaired kidney function can lead to abnormalities in bone metabolism, including decreased bone mineral density and increased fracture risk.
The kidneys play a crucial role in maintaining mineral balance and regulating vitamin D metabolism, both of which are essential for bone health. In individuals with diabetic nephropathy, these processes are disrupted, leading to bone complications.
Preventive Measures and Treatments
While bone health complications are a significant concern for people with diabetes, several preventive measures and treatments can help maintain and improve bone health:.
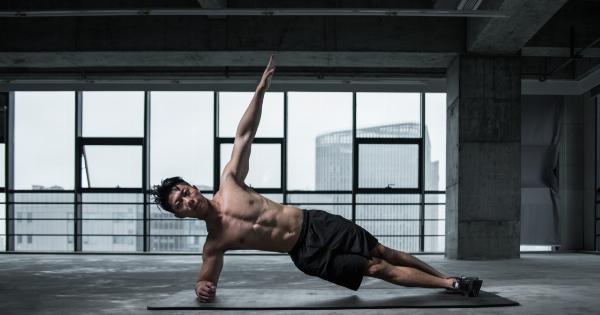
a) Regular exercise: Engaging in weight-bearing exercises, such as walking, jogging, or strength training, can promote bone density and reduce the risk of fractures.
Exercise also improves insulin sensitivity and glycemic control, benefiting overall diabetes management.
b) Adequate vitamin D and calcium intake: Ensuring sufficient intake of vitamin D and calcium is crucial for bone health.
Vitamin D can be obtained through sunlight exposure and dietary sources, while calcium-rich foods include dairy products, green leafy vegetables, and fortified foods. Supplementation may be necessary if dietary intake is insufficient.
c) Optimal glycemic control: Maintaining optimal blood glucose levels is essential for preserving bone health. Consistently high blood sugar levels can impair bone formation and increase the risk of complications.
Consultation with a healthcare professional is crucial for individualized glycemic management.
d) Medication review: Regular review of diabetes medications is important to assess their potential impact on bone health. If a medication is found to negatively affect bone density, alternative options can be explored with healthcare providers.
Conclusion
Diabetes poses significant challenges to bone health, increasing the risk of complications such as osteoporosis, fractures, foot ulcers, and amputation.
Understanding the underlying mechanisms and implementing preventive measures are crucial in mitigating these risks. Regular exercise, maintaining optimal glycemic control, and ensuring adequate intake of vitamin D and calcium play vital roles in preserving bone health.
It is essential for individuals with diabetes to work closely with healthcare professionals to develop personalized strategies for managing their diabetes while also safeguarding their bone health.