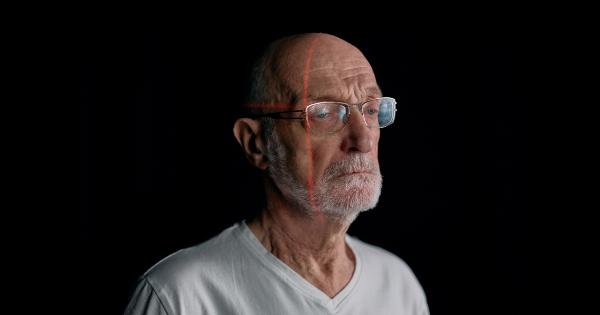
Eye rejection, also known as ocular rejection, is a complex immunological response in which the body’s immune system mounts an attack against a transplanted cornea or other eye tissue.
This rejection process involves a series of inflammatory reactions that can lead to a loss of vision and potential complications. Understanding the causes of eye rejection is critical for improving transplantation success rates and developing strategies to prevent or treat this condition.
Immunological Factors
One of the primary causes of eye rejection is the mismatch between the donor tissue and the recipient’s immune system. The immune response is triggered by the recognition of foreign antigens present on the transplanted tissue.
Various immune cell types participate in this process, including T cells, B cells, and macrophages.
T-cell Mediated Rejection
T-cell mediated rejection is the most common form of eye rejection. When T cells recognize foreign antigens on the transplanted tissue, they release cytokines that recruit and activate other immune cells.
This process leads to inflammation and can result in damage to the cornea. The severity of T-cell mediated rejection varies but can lead to corneal graft failure if left untreated.
Endothelial Rejection
Endothelial rejection specifically targets the endothelial cells lining the inside of the cornea. It is typically characterized by the presence of corneal endothelial deposits known as Khodadoust line.
This type of rejection is often associated with a history of previous corneal transplants and high-risk individuals.
Humoral Rejection
Humoral rejection, also known as antibody-mediated rejection, occurs when antibodies produced by the recipient’s immune system target antigens on the transplanted tissue. This can lead to complement activation, inflammation, and tissue damage.
Humoral rejection is less common than T-cell mediated rejection but can have severe consequences if not promptly treated.
HLA Matching
Human leukocyte antigen (HLA) matching plays a crucial role in eye transplant success. HLA molecules are proteins that regulate immune responses and are highly polymorphic, meaning they vary between individuals.
The closer the HLA match between donor and recipient, the lower the risk of rejection. HLA matching is typically performed before transplantation to identify compatible donors, but even with a good match, the risk of rejection is not completely eliminated.
Corneal Transplantation Techniques
The surgical techniques used during corneal transplantation can also influence the risk of eye rejection.
Penetrating keratoplasty, where the entire thickness of the cornea is replaced, has a higher rejection rate compared to partial-thickness procedures such as lamellar keratoplasty. The difference is believed to be related to the increased antigenic load presented by full-thickness transplants.
Recurrent Herpes Simplex Virus (HSV) Infections
Individuals with a history of recurrent herpes simplex virus (HSV) infections, especially ocular herpes, have an increased risk of eye rejection following corneal transplantation.
The underlying immunological changes caused by HSV infection can lead to an exaggerated immune response against the transplanted tissue.
Prevention and Treatment
Preventing eye rejection involves a combination of preoperative assessment, careful donor selection, and postoperative immunosuppression.
Medications such as corticosteroids, cyclosporine, and tacrolimus are commonly used to suppress the immune response and reduce the risk of rejection. Regular monitoring and follow-up visits are necessary to detect signs of rejection early and provide timely treatment.
Future Directions
Ongoing research aims to develop improved immunosuppressive strategies, increase understanding of the factors contributing to eye rejection, and identify potential biomarkers for early detection.
Advancements in tissue engineering and regenerative medicine may also lead to the development of alternative treatment options that eliminate the need for donor tissue altogether, reducing the risk of rejection.
Conclusion
Eye rejection remains a significant challenge in the field of corneal transplantation. A better understanding of the causes of rejection and the immune mechanisms involved is essential for improving transplant outcomes and developing targeted therapies.
By addressing immunological factors, improving surgical techniques, and implementing appropriate preventive measures, researchers strive to enhance the success rates of corneal transplantation and ultimately improve the quality of life for patients with vision loss.