Idiopathic hypertension, also known as essential hypertension, is a common medical condition characterized by high blood pressure with no identifiable cause.
It affects a significant portion of the global population and is a major risk factor for cardiovascular diseases such as heart attack and stroke. While several environmental and lifestyle factors contribute to the development of hypertension, research has increasingly recognized the role of genetics in determining an individual’s susceptibility to idiopathic hypertension.
In this article, we will explore the relationship between genetics and idiopathic hypertension, highlighting the genetic variants and pathways that have been implicated in its pathogenesis.
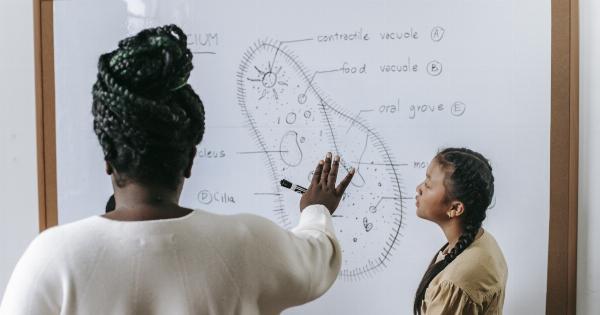
Genetics and Hypertension
Hypertension has long been recognized as a multifactorial disease, influenced by a combination of genetic and environmental factors.
Familial aggregation studies have provided strong evidence for a genetic component in hypertension, showing that individuals with a family history of hypertension are more likely to develop the condition than those without such a history. Additionally, the heritability of hypertension, estimated through twin and family studies, suggests that genetic factors may account for up to 50% of the variation in blood pressure levels among individuals.
Single Gene Variants
While idiopathic hypertension is a complex genetic disorder influenced by numerous genes, some single gene variants have been identified that play a significant role in its development.
One of the most well-known examples is mutations in the gene encoding the angiotensin converting enzyme (ACE). These mutations result in increased production of angiotensin II, a potent vasoconstrictor that raises blood pressure. The presence of the ACE gene variants has been associated with higher blood pressure levels and an increased risk of hypertension.
Hypertension-Associated Genetic Pathways
In addition to single gene variants, research has also identified several genetic pathways and mechanisms that contribute to the development of hypertension. One such pathway involves the regulation of salt and water balance by the kidneys.
Genetic variants in genes encoding proteins involved in renal sodium reabsorption, such as the sodium-chloride cotransporter (NCC) and the epithelial sodium channel (ENaC), have been associated with increased blood pressure and hypertension risk. Dysfunction in these pathways can lead to excessive sodium retention and volume expansion, ultimately leading to elevated blood pressure.
Role of the Renin-Angiotensin System
The renin-angiotensin system (RAS) is a hormonal pathway involved in the regulation of blood pressure and fluid balance. It is primarily controlled by the action of angiotensin-converting enzyme (ACE), which converts angiotensin I to angiotensin II.
Genetic variants in genes encoding ACE and other components of the RAS pathway, such as angiotensinogen (AGT) and angiotensin receptor type 1 (AGTR1), have been associated with hypertension susceptibility. These variants can influence the production and activity of angiotensin II, leading to increased vasoconstriction and blood pressure elevation.
Epigenetics and Hypertension
In recent years, the field of epigenetics has emerged as an important area of research in understanding the genetic underpinnings of hypertension.
Epigenetic modifications, such as DNA methylation and histone acetylation, can alter gene expression without changing the underlying DNA sequence. Studies have shown that epigenetic changes in genes related to blood pressure regulation, such as the RAS pathway, can contribute to the development of hypertension.
Environmental factors, such as diet and stress, can influence these epigenetic modifications, further highlighting the interplay between genetics and the environment in hypertension.
Genome-Wide Association Studies
In recent years, advances in genomic technology have enabled large-scale studies to identify genetic variants associated with complex diseases like hypertension.
Genome-wide association studies (GWAS) have identified numerous genetic loci associated with blood pressure and hypertension risk. These loci often reside in regions near genes involved in cardiovascular physiology and regulation of blood pressure.
While the individual effects of these variants might be small, collectively they contribute to the overall risk of developing hypertension.
Gene-Environment Interactions
It is important to recognize that genetics alone does not determine an individual’s risk of hypertension. Gene-environment interactions play a critical role in modulating disease risk.
For example, an individual with a genetic predisposition for hypertension may be more susceptible to developing the condition if exposed to dietary factors high in sodium or a sedentary lifestyle. Conversely, individuals with a low genetic risk may still develop hypertension if exposed to certain environmental risk factors. Understanding these gene-environment interactions can help inform personalized prevention and treatment strategies.
Targeting Genetics for Hypertension Management
The growing body of research on the genetics of hypertension offers promising opportunities for the development of targeted therapies.
By identifying specific genetic variants or pathways associated with hypertension, researchers hope to develop novel drugs that can modulate these targets and lower blood pressure. This personalized approach to treatment could potentially improve the effectiveness and reduce the side effects associated with current antihypertensive medications.
However, further research is needed to fully elucidate the complex genetic architecture of hypertension and translate these findings into clinical practice.
Conclusion
Idiopathic hypertension is a complex disorder with multiple genetic and environmental factors contributing to its development.
While numerous genetic variants and pathways have been implicated in hypertension, our understanding of its genetic underpinnings is still evolving. By exploring the relationship between genetics and idiopathic hypertension, researchers aim to improve risk prediction, early detection, and treatment strategies for this prevalent condition.
With ongoing advancements in genetic research and precision medicine, the future holds promise for more targeted and individualized approaches to hypertension management.