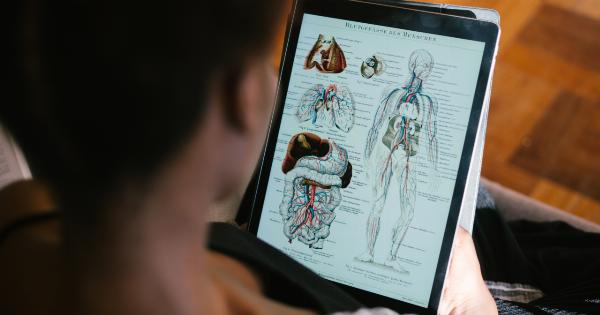
Endometritis is a common gynecological condition that affects women of reproductive age. It refers to the inflammation of the endometrium, which is the lining of the uterus.
This condition can have a significant impact on a woman’s reproductive system and can cause various symptoms and complications. In this article, we will delve into the details of how endometritis affects a woman’s reproductive system.
Understanding Endometritis
Endometritis occurs when bacteria or other pathogens enter the uterus and cause an infection. The most common cause of endometritis is the ascent of bacteria from the vagina or cervix into the uterus.
This can happen during childbirth, medical procedures involving the uterus, or sexual intercourse. Other risk factors for developing endometritis include a weakened immune system, a history of pelvic inflammatory disease (PID), or the use of an intrauterine device (IUD).
Endometritis can be classified as acute or chronic, depending on the duration and severity of the inflammation. Acute endometritis is characterized by sudden onset symptoms and is usually caused by an infection.
Chronic endometritis, on the other hand, is a long-standing inflammation of the endometrium and may be associated with other underlying conditions such as endometriosis or fibroids.
Symptoms of Endometritis
The symptoms of endometritis may vary depending on the severity and duration of the infection. Some common symptoms include:.
- Abnormal vaginal bleeding
- Pain or discomfort in the lower abdomen
- Fever and chills
- Abnormal vaginal discharge with a foul odor
- Painful sexual intercourse
- General fatigue and malaise
If you experience any of these symptoms, it is important to seek medical attention promptly as untreated endometritis can lead to complications and further damage to the reproductive system.
Impact on Fertility
Endometritis can have a significant impact on a woman’s fertility. The infection and inflammation can affect the normal functioning of the endometrium, making it less receptive to implantation and pregnancy.
The presence of bacterial pathogens can also directly damage the developing embryo, leading to a higher risk of miscarriage.
In addition to affecting the endometrium, endometritis can also cause scarring and adhesions in the reproductive organs. These adhesions can block the fallopian tubes, preventing the egg from meeting the sperm and resulting in infertility.
Furthermore, chronic inflammation in the reproductive system can disrupt the delicate hormonal balance necessary for ovulation and the menstrual cycle, further impairing fertility.
Complications of Endometritis
If left untreated, endometritis can lead to several complications that can have long-term effects on a woman’s reproductive health. Some of the complications include:.
- Chronic pelvic pain: The chronic inflammation associated with endometritis can cause persistent pelvic pain.
- Infertility: As mentioned earlier, endometritis can impair fertility due to damage to the endometrium and fallopian tubes.
- Septicemia: In severe cases, the infection can spread to the bloodstream, resulting in a condition called septicemia, which can be life-threatening.
- Increased risk of ectopic pregnancy: The presence of adhesions and tubal blockages can increase the risk of ectopic pregnancy, where the fertilized egg implants outside the uterus.
It is crucial to diagnose and treat endometritis promptly to prevent these complications from occurring.
Diagnosis of Endometritis
If you experience symptoms suggestive of endometritis, your healthcare provider will perform a thorough evaluation to make a definitive diagnosis. The diagnostic process may include:.
- Medical history: Your doctor will inquire about your symptoms, medical history, and any risk factors that might contribute to the development of endometritis.
- Physical examination: A pelvic examination will be conducted to check for any signs of infection or inflammation in the reproductive organs.
- Lab tests: A sample of vaginal discharge or cervical mucus may be taken to identify the specific bacteria causing the infection.
- Imaging tests: In some cases, imaging tests such as ultrasound or MRI may be ordered to assess the extent of inflammation or to detect any structural abnormalities.
- Endometrial biopsy: A small sample of the endometrium may be obtained for microscopic analysis to confirm the diagnosis of endometritis.
Once the diagnosis is confirmed, appropriate treatment can be initiated to manage the infection and prevent further complications.
Treatment for Endometritis
The primary treatment for endometritis is a course of antibiotics to eliminate the infection. The specific choice of antibiotics will depend on the type of bacteria causing the infection and its sensitivity to certain medications.
In severe cases or cases with an abscess, hospitalization and intravenous antibiotics may be necessary.
It is crucial to complete the full course of antibiotics as prescribed by your healthcare provider to ensure complete eradication of the infection. Failure to do so may lead to recurrent infections or the development of antibiotic resistance.
In addition to antibiotics, pain medication may be prescribed to alleviate any discomfort or pelvic pain associated with endometritis. Bed rest and adequate hydration are also recommended during the recovery process.
Prevention of Endometritis
While it may not be possible to prevent all cases of endometritis, there are certain measures that can be taken to reduce the risk:.
- Maintaining good hygiene: Practicing good genital hygiene can help prevent the ascent of bacteria into the uterus. This includes regular washing of the external genital area and using clean sanitary products.
- Safe sexual practices: Using barrier methods such as condoms can reduce the risk of sexually transmitted infections that can lead to endometritis.
- Early treatment of pelvic infections: Prompt diagnosis and treatment of conditions such as bacterial vaginosis or PID can help prevent the spread of infection to the uterus.
- Proper care during childbirth and medical procedures: Ensuring proper sterilization and adherence to aseptic techniques during childbirth and medical procedures involving the uterus can reduce the risk of infection.
By following these preventive measures, the chances of developing endometritis can be significantly reduced.
Conclusion
Endometritis is a condition that can have a profound impact on a woman’s reproductive system.
It can cause symptoms such as abnormal vaginal bleeding, abdominal pain, and fever, and can lead to complications such as infertility and chronic pelvic pain if left untreated. Prompt diagnosis and appropriate treatment with antibiotics are essential to manage the infection and prevent further damage to the reproductive organs.
Additionally, practicing good hygiene, safe sexual practices, and seeking early treatment for pelvic infections can help reduce the risk of developing endometritis and its associated complications.