Infarction, commonly known as a heart attack, is a life-threatening condition that occurs when the blood supply to a part of the heart is interrupted, leading to tissue damage and potential organ failure.
It is a major cause of death globally and can be triggered by various factors, including the presence of respiratory infections. This article aims to explore the relationship between respiratory infections and the risk of infarction.
The Link Between Respiratory Infections and Infarction
Research studies have indicated a significant association between respiratory infections and an increased risk of infarction.
Respiratory infections, such as influenza and pneumonia, can lead to systemic inflammation and trigger an immune response that promotes the development of arterial plaques. These plaques, composed of cholesterol, fatty deposits, and cellular waste products, can obstruct blood flow and increase the likelihood of infarction.
Inflammation and Atherosclerosis
Respiratory infections cause an upregulation of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α).
These cytokines contribute to the inflammatory response, leading to endothelial dysfunction and an increased risk of plaque formation. In addition, the body’s immune response to infections can trigger the release of C-reactive protein (CRP), an established marker of inflammation and a predictor of cardiovascular events.
Infectious Agents and Cardiovascular Risk
Certain infectious agents have been implicated in the development of infarction by promoting atherosclerosis. For example, studies have identified a link between Chlamydia pneumoniae infection and the progression of atherosclerosis.
The presence of this bacterium in arterial plaques suggests a direct role in the development and destabilization of these structures, ultimately increasing the risk of infarction.
Immune Response and Plaque Stability
The immune response to respiratory infections can also influence plaque stability. When the body fights off an infection, immune cells accumulate in arterial walls, leading to the production of metalloproteinases.
These enzymes can degrade the collagen fibers of a plaque, weakening its structure and increasing the likelihood of rupture. Plaque rupture exposes the bloodstream to thrombogenic substances, which can result in a complete blockage of blood flow and cause an infarction.
Prevention and Management Strategies
Given the association between respiratory infections and infarction risk, preventive strategies should be emphasized.
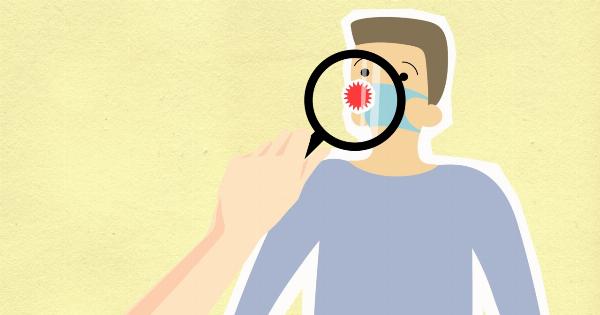
Vaccination against common respiratory pathogens, such as influenza and Streptococcus pneumoniae, can significantly reduce the incidence of respiratory infections and consequently lower the risk of infarction. Encouraging good respiratory hygiene, such as handwashing and avoiding close contact with infected individuals, can also be effective preventive measures.
In terms of management, prompt and appropriate treatment of respiratory infections is crucial. Timely administration of antiviral or antibiotic therapies can help control the infection, minimize inflammation, and reduce the risk of infarction.
Additionally, healthcare providers should be vigilant in monitoring and managing cardiovascular risk factors, such as high blood pressure and high cholesterol, in individuals with respiratory infections.
Conclusion
Respiratory infections play a significant role in increasing the risk of infarction.
The associated systemic inflammation and immune responses can contribute to the development and destabilization of arterial plaques, ultimately leading to the obstruction of blood flow and the occurrence of infarction. Emphasizing preventive measures, such as vaccination and respiratory hygiene, along with appropriate management strategies, is crucial in mitigating the impact of respiratory infections on infarction risk.