Gastroesophageal Reflux Disease (GERD) is a chronic digestive condition that affects millions of people worldwide.
It occurs when the stomach acid and other digestive juices flow back into the esophagus, causing symptoms such as heartburn, chest pain, regurgitation, and difficulty swallowing. While lifestyle changes, medication, and other non-surgical treatments can often help manage GERD symptoms, some patients may require surgical intervention for long-term relief.
What is Minimally Invasive GERD Surgery?
Minimally invasive GERD surgery refers to surgical techniques that are performed using small incisions and specialized instruments.
These procedures aim to correct the underlying anatomical issues causing GERD, such as a hiatal hernia or a weak lower esophageal sphincter (LES). The minimally invasive approach offers several advantages over traditional open surgery, including reduced pain, shorter hospital stays, faster recovery times, and smaller scars.
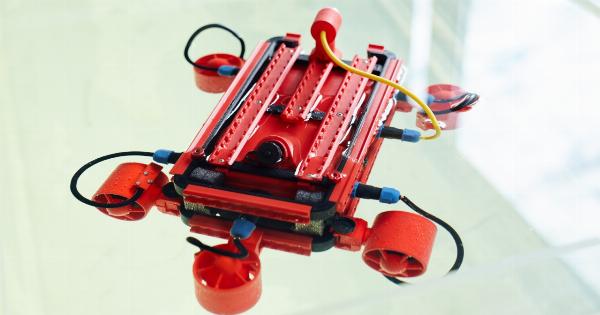
Enter Robotics in GERD Surgery
Robotic-assisted surgery has revolutionized many fields of medicine, and GERD surgery is no exception. Robot-assisted surgery provides surgeons with enhanced precision, dexterity, and control, allowing for highly accurate and efficient procedures.
The robotic system consists of robotic arms controlled by the surgeon, a high-definition 3D camera for visualization, and specialized instruments that mimic human wrist movements.
The Benefits of Robotic GERD Surgery
1. Enhanced Precision: Robotic systems offer a greater range of motion and more precise movements, enabling surgeons to navigate intricate anatomical structures with improved accuracy.
This precision contributes to better surgical outcomes and reduced risk of complications.
2. Faster Recovery: Minimally invasive robotic surgery typically results in less trauma to the tissues, reduced blood loss, and minimal scarring.
This allows patients to experience a faster recovery, with shorter hospital stays and a quicker return to their normal activities.
3. Reduced Complications: The advanced technology and enhanced visualization provided by robotic-assisted surgery help minimize the risk of complications during GERD procedures.
Surgeons can better identify and address underlying issues like hiatal hernias or LES weaknesses while avoiding damage to surrounding healthy tissues.
4. Personalized Approach: Robotic technology allows surgeons to tailor the procedure to each patient’s unique anatomy.
The instruments used in robotic-assisted surgery can adapt to varying tissue thicknesses and spatial constraints, ensuring a personalized and optimal surgical experience.
The Role of Robotic-Assisted Fundoplication
Fundoplication is a surgical procedure commonly used to treat GERD.
During fundoplication, the surgeon wraps the upper part of the stomach (fundus) around the lower esophagus, reinforcing the LES and preventing stomach acid from refluxing into the esophagus. Robotic-assisted fundoplication offers additional advantages in comparison to traditional laparoscopic fundoplication:.
High-definition Visualization
The robotic system provides surgeons with a high-definition, magnified, 3D view of the surgical field.
This enhanced visualization enables clear identification of anatomical structures and precise placement of sutures, ensuring an accurate and effective fundoplication.
Better Ergonomics for Surgeons
The robotic surgical system offers improved ergonomics compared to traditional laparoscopic surgery. Surgeons can operate from a comfortable console, utilizing ergonomic hand controls and foot pedals to direct the robotic arms.
This enhanced ergonomics reduce the physical strain on surgeons, leading to improved precision and reduced fatigue during prolonged procedures.
Patient Selection for Minimally Invasive GERD Surgery
While minimally invasive GERD surgery with robotics offers numerous benefits, not all patients are suitable candidates for these procedures.
Factors such as overall health, severity of GERD symptoms, anatomical abnormalities, and previous surgical history may influence the decision to opt for robotic-assisted surgery. A thorough evaluation by a gastroenterologist or a specialist surgeon specializing in GERD treatment is necessary to determine the appropriate surgical approach for each patient.
Potential Risks and Complications
As with any surgical procedure, there are potential risks and complications associated with minimally invasive GERD surgery.
These may include infection, bleeding, allergic reactions to anesthesia, injury to surrounding organs or structures, and the possibility of hernia recurrence. However, the advancement of robotic-assisted techniques has significantly reduced the occurrence of such complications.
Conclusion
Minimally invasive GERD surgery with robotics offers a wide range of benefits over traditional open surgery and even laparoscopic procedures.
The precision and personalized approach of robotic-assisted surgery contribute to improved outcomes, faster recoveries, and reduced complications for patients suffering from GERD. By leveraging the capabilities of robotic systems, surgeons can provide effective, long-term relief to patients, allowing them to enjoy an improved quality of life.