Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). It is spread through sexual contact and can be transmitted even if there are no visible sores or symptoms.
Genital herpes can have significant physical and emotional effects on those who contract it, but there are ways to minimize complications and manage the infection.
Understanding HSV-1 and HSV-2
There are two types of herpes simplex virus: HSV-1 and HSV-2. HSV-1 typically causes oral herpes, such as cold sores around the mouth, while HSV-2 primarily causes genital herpes.
However, both types can infect the genital area and oral area through different modes of transmission. HSV-2 is more commonly associated with genital herpes, but it is possible to contract genital herpes from HSV-1 through oral sex.
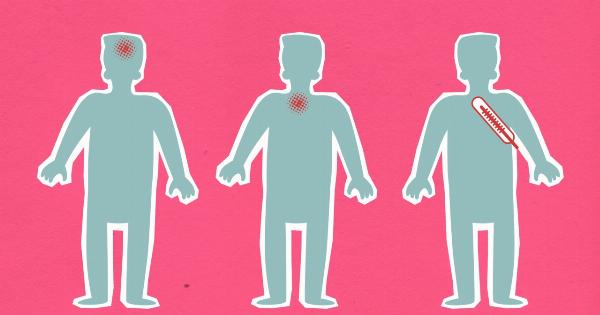
Common Symptoms of Genital Herpes
Genital herpes can cause a range of symptoms, although many individuals infected with HSV may not experience any noticeable symptoms. When symptoms do occur, they can include:.
- Painful blisters or sores in the genital or anal area
- Itching or tingling sensation before the blisters appear
- Pain or burning during urination
- Flu-like symptoms, such as fever, headache, and swollen glands
- General discomfort and body aches
Complications and Risks
While genital herpes itself is not life-threatening, it can lead to several complications and pose risks to both the infected individual and their sexual partners. Some common complications associated with genital herpes include:.
- Increased risk of acquiring other STIs: Genital herpes can make it easier for an individual to contract other sexually transmitted infections, including HIV.
- Pregnancy complications: Pregnant individuals with genital herpes may transmit the virus to their baby during childbirth, potentially leading to severe complications or even death.
- Increased risk of cervical cancer: Studies have shown a potential link between HSV-2 infection and an increased risk of developing cervical cancer.
- Emotional and psychological impacts: The diagnosis of genital herpes can have a significant emotional impact, leading to feelings of shame, guilt, anxiety, and depression.
Prevention Strategies
Although there is no cure for genital herpes, there are several prevention strategies that can help minimize the risk of transmission and reduce complications:.
- Practice safe sex: Consistently using condoms or dental dams during sexual activities can significantly reduce the risk of transmitting genital herpes.
- Avoid sexual contact during outbreaks: It is important to abstain from sexual activities when visible symptoms or sores are present to avoid transmitting the virus.
- Discuss HSV status with partners: Openly communicating about herpes and STI status with sexual partners can help make informed decisions regarding sexual activities.
- Take antiviral medication: Antiviral medications can reduce the frequency and severity of outbreaks, as well as the risk of transmission to sexual partners.
- Get vaccinated for other STIs: Vaccines are available for some sexually transmitted infections, such as HPV, which can reduce the risk of complications associated with multiple infections.
Managing Outbreaks
While preventing outbreaks entirely may not be possible, there are measures individuals with genital herpes can take to manage and minimize the impact of outbreaks:.
- Seek medical advice: Consult a healthcare provider for proper diagnosis, treatment, and ongoing management of genital herpes. They may prescribe antiviral medications or recommend lifestyle changes to help manage outbreaks.
- Practice good hygiene: Keep the affected area clean and dry to prevent the spread of infection and reduce irritation. Avoid scratching or touching the sores to prevent further complications.
- Avoid triggers: Certain factors can trigger herpes outbreaks, including stress, illness, and hormonal changes. Identify and avoid these triggers to reduce the frequency and severity of outbreaks.
- Manage stress: Incorporate stress-reducing techniques, such as exercise, meditation, and therapy, into daily life to minimize the impact of stress on the immune system and outbreaks.
- Support and counseling: Seek support from healthcare professionals, support groups, or counseling services to cope with the emotional and psychological aspects of living with genital herpes.
Reducing Stigma and Seeking Support
Living with genital herpes can be emotionally challenging due to the stigma associated with the infection. It is essential to understand that herpes is a common and manageable condition.
Seeking support from healthcare professionals, counselors, or support groups can help individuals cope with the emotional aspects and provide valuable information.
Conclusion
While genital herpes can have complications and impacts, there are effective strategies to minimize its effects.
Practicing safe sex, discussing HSV status with partners, taking antiviral medications, and managing outbreaks can reduce the risk of transmission and improve the overall quality of life for individuals with genital herpes. Seeking support and understanding can also play a significant role in coping with the emotional aspects of living with this infection.