Obesity is a serious health issue that affects millions of people worldwide. According to the World Health Organization (WHO), obesity is defined as having a body mass index (BMI) equal to or greater than 30.
BMI is calculated by dividing a person’s weight in kilograms by their height in meters squared.
The prevalence of obesity has been steadily increasing in the past few decades.
A report by the Centers for Disease Control and Prevention (CDC) states that in the United States, the prevalence of obesity was 42.4% in 2018, an increase from 30.5% in 1999.
Obesity is linked to several health problems, including heart disease, diabetes, and high blood pressure. However, the effects of obesity on brain health are also becoming a growing concern.
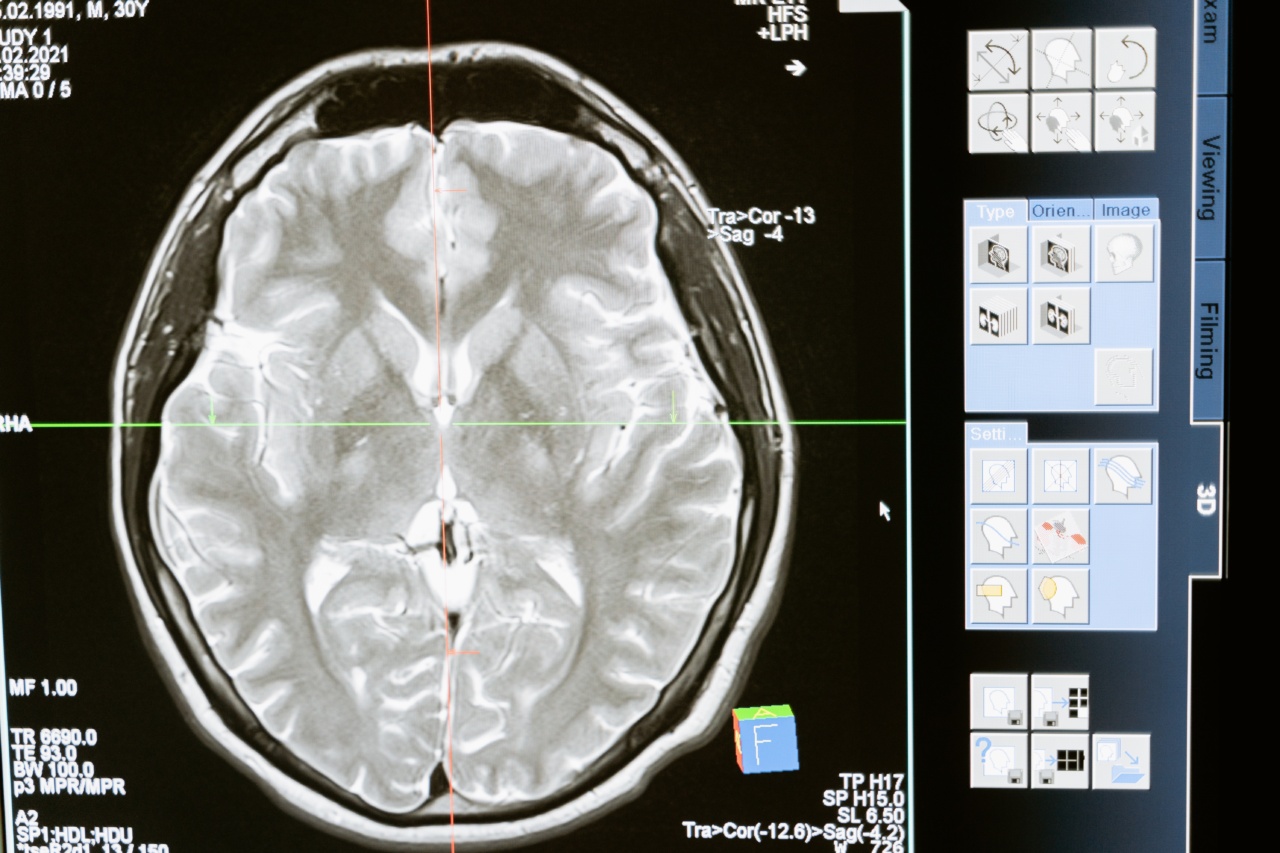
Obesity and Brain Structure
Obesity has been linked to changes in brain structure, particularly in the gray and white matter.
A study published in the journal Radiology found that obese individuals had lower gray matter volumes in certain areas of the brain, including the frontal and temporal lobes, compared to non-obese individuals. Gray matter is responsible for processing information in the brain.
Another study published in the Journal of Alzheimer’s Disease found that obese individuals had reduced white matter integrity in the corpus callosum, a bundle of nerve fibers that connect the two hemispheres of the brain.
White matter is responsible for communication between different areas of the brain.
Obesity and Cognitive Function
Several studies have investigated the relationship between obesity and cognitive function. A meta-analysis published in the journal Obesity Reviews found that obese individuals performed worse on cognitive tests compared to non-obese individuals.
The study also found that the negative effects of obesity on cognitive function were more pronounced in middle-aged and elderly individuals.
Another study published in the journal JAMA Neurology found that midlife obesity was associated with worse cognitive function in later life.
The study followed participants over a period of 32 years and found that those who were obese in midlife had lower cognitive scores in later life compared to those who were not obese.
Obesity and Dementia
Dementia is a progressive neurodegenerative disorder that affects memory, thinking, and behavior. It is a major cause of disability and dependency in older adults. Several studies have investigated the relationship between obesity and dementia.
A study published in the journal Neurology found that obese individuals were more likely to develop dementia compared to non-obese individuals.
The study followed participants over a period of 36 years and found that those who were obese in midlife had a 74% higher risk of developing dementia compared to those who were not obese.
Another study published in the journal JAMA Psychiatry found that midlife obesity was associated with increased risk of dementia in women but not in men.
The study followed participants over a period of 40 years and found that women who were obese in midlife had a 21% higher risk of developing dementia compared to those who were not obese.
Obesity and Depression
Depression is a common mental health disorder that affects millions of people worldwide. Several studies have investigated the relationship between obesity and depression.
A meta-analysis published in the journal Obesity Reviews found that obese individuals were more likely to develop depression compared to non-obese individuals.
The study also found that the risk of depression was higher in individuals who had been obese for longer periods of time.
Another study published in the journal JAMA Psychiatry found that midlife obesity was associated with increased risk of depression in later life.
The study followed participants over a period of 40 years and found that those who were obese in midlife had a higher risk of developing depression in later life compared to those who were not obese.
Obesity and Sleep Disorders
Sleep disorders are a common problem among obese individuals. Obstructive sleep apnea (OSA) is a sleep disorder characterized by repeated breathing interruptions during sleep. Several studies have investigated the relationship between obesity and OSA.
A meta-analysis published in the journal Chest found that obese individuals were more likely to develop OSA compared to non-obese individuals. The study also found that the severity of OSA was higher in obese individuals.
Another study published in the journal Sleep Medicine Reviews found that weight loss was effective in reducing the severity of OSA in obese individuals. The study also found that weight loss improved symptoms of OSA, such as daytime sleepiness.
Obesity and Brain Function
Obesity has been linked to changes in brain function, particularly in areas related to reward and motivation.
A study published in the journal JAMA Psychiatry found that obese individuals had reduced function in the striatum, an area of the brain that is involved in reward processing and motivation. The study also found that the negative effects of obesity on striatal function were more pronounced in individuals who were insulin-resistant.
Another study published in the journal Proceedings of the National Academy of Sciences found that obese individuals had reduced connectivity between the ventromedial prefrontal cortex and the striatum.
The ventromedial prefrontal cortex is involved in decision-making processes.
Conclusion
Obesity is a serious health issue that affects millions of people worldwide. The negative effects of obesity on brain health are becoming a growing concern.
Obesity has been linked to changes in brain structure, cognitive function, dementia, depression, sleep disorders, and brain function. It is important to address the issue of obesity to improve overall health and prevent negative effects on brain health.