As the global population continues to age, the prevalence of pain among geriatric patients is becoming a significant concern. Older adults often suffer from chronic conditions that cause persistent pain, such as arthritis, cancer, and neuropathy.
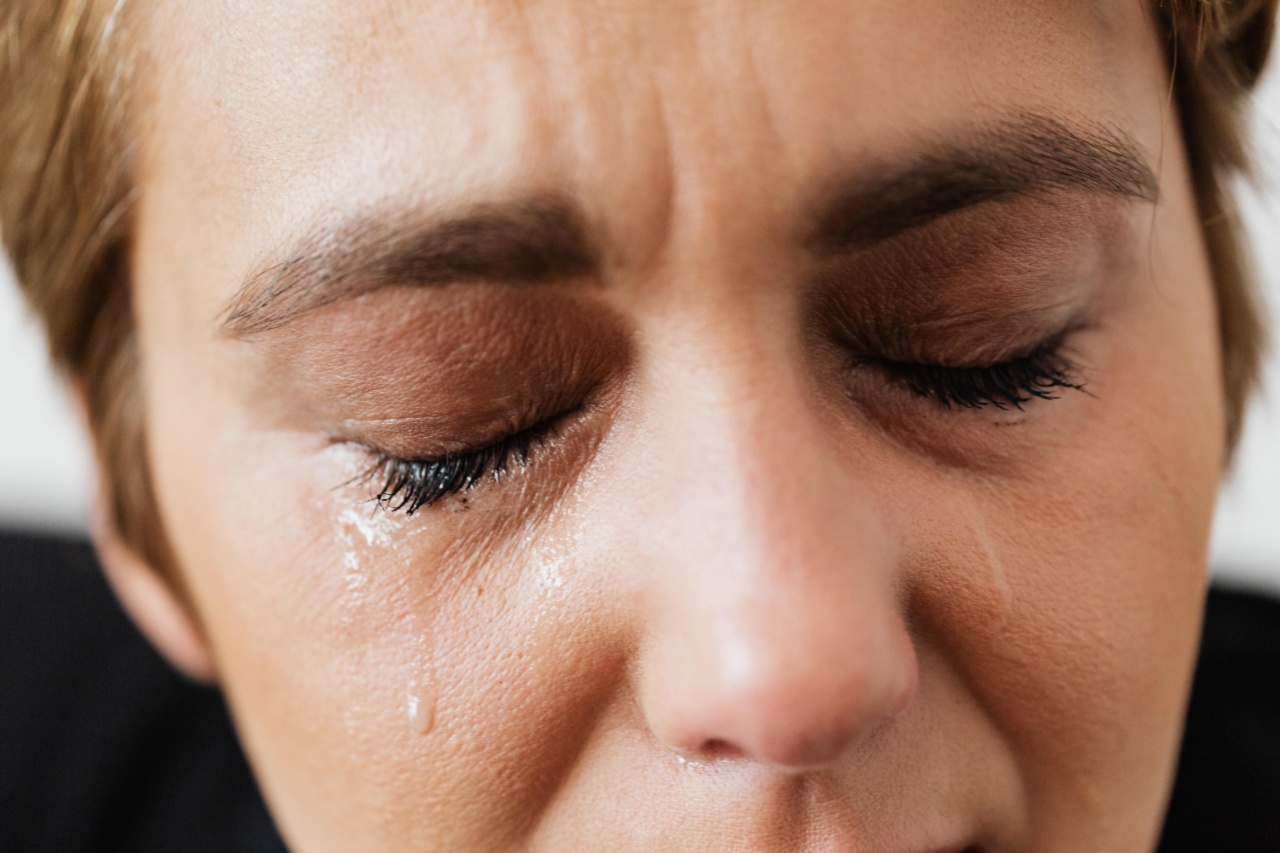
The impact of unmanaged pain on their overall well-being and quality of life cannot be overlooked. In this article, we will explore the unique challenges faced in pain management for geriatric patients and discuss strategies to improve their comfort and alleviate suffering.
The Complexities of Pain in the Elderly
Geriatric patients experience pain differently from younger individuals due to various physiological and psychological factors.
Age-related changes in the body, including decreased tissue elasticity, impaired wound healing, and the presence of comorbidities, contribute to altered pain perception and tolerance. Furthermore, cognitive decline, memory impairment, and communication barriers in the elderly population can complicate the assessment and management of pain.
Barriers to Effective Pain Management in Geriatrics
Pain management in geriatric patients is often challenging due to several barriers that healthcare professionals must navigate:.
1. Underreporting of Pain
Elderly individuals may be reluctant to report pain due to a fear of dependence on medications, concerns about side effects, or a belief that pain is an inevitable part of aging.
It is crucial for healthcare providers to actively inquire about pain and create a safe and trusting environment that encourages open communication.
2. Polypharmacy
The elderly population often juggles multiple medications for various chronic illnesses. Polypharmacy can increase the risk of drug-drug interactions and side effects, complicating pain management.
Close monitoring and regular medication reviews are essential to optimize pain relief while minimizing adverse effects.
3. Cognitive Impairment
Cognitive decline can make it challenging for geriatric patients to accurately express their pain intensity, duration, or location.
Healthcare providers should employ alternative pain assessment tools, such as observing behavioral changes, facial expressions, or vocalizations, to better evaluate pain in patients with cognitive impairment.
4. Inadequate Education
Both patients and healthcare providers may have limited knowledge about pain management in the elderly.
Educational initiatives aimed at improving pain assessment, treatment options, and non-pharmacological interventions for geriatric patients are crucial to enhance pain management outcomes.
Strategies for Improved Pain Management
Addressing the unique challenges of pain management in geriatric patients requires a multifaceted approach. Here are some strategies that can contribute to better pain control and overall well-being for older adults:.
1. Comprehensive Assessment
A thorough assessment is the cornerstone of effective pain management. It should include a detailed medical history, a review of current medications, a physical examination, and a pain assessment using validated tools.
Taking into account the patient’s cultural and individual preferences is vital to tailor treatment plans accordingly.
2. Individualized Treatment Plans
Geriatric patients require personalized treatment plans considering their comorbidities, medication regimen, cognitive function, and overall goals of care.
A multi-modal approach that incorporates pharmacological and non-pharmacological interventions, such as physical therapy, cognitive-behavioral therapy, and acupuncture, can optimize pain relief while minimizing drug-related risks.
3. Regular Medication Reviews
Periodic evaluations of medication regimens, including pain medications, can help identify any redundancies, interactions, or potential side effects.
Collaborative efforts between healthcare providers and pharmacists can ensure optimal analgesic use and minimize polypharmacy-related issues.
4. Patient Education
Providing education to geriatric patients about their pain condition, treatment options, and potential side effects is crucial for informed decision-making.
Clear instructions on medication use, adherence, and non-pharmacological interventions empower elderly individuals to actively participate in their pain management.
5. Multidisciplinary Collaboration
Collaboration among healthcare professionals, including physicians, nurses, pharmacists, physical therapists, and psychologists, is vital to address the complex needs of geriatric patients.
A multidisciplinary approach allows for holistic care that targets not only pain management but also other aspects of well-being, such as mobility, mental health, and social support.
6. Palliative Care and Hospice Services
In cases where curative treatment is no longer an option, palliative care and hospice services play a crucial role in providing comfort and pain relief for geriatric patients.
These specialized services focus on improving the quality of life by addressing not only physical pain but also emotional, social, and spiritual distress.
Conclusion
The management of pain in geriatric patients is a pressing concern as the aging population continues to grow.
By recognizing the complexities and barriers associated with pain management in the elderly, healthcare providers can implement strategies that improve the quality of life for older adults.
Comprehensive assessments, individualized treatment plans, medication reviews, patient education, multidisciplinary collaboration, and access to palliative care services are essential components of an effective pain management approach for geriatric patients. By addressing these challenges head-on, we can strive to alleviate suffering and ensure the well-being of our aging population.