Parkinson’s disease is a progressive neurological disorder that affects millions of people worldwide.
Currently, there is no known cure for this debilitating condition, making early detection and intervention crucial for managing its symptoms and improving patients’ quality of life. However, traditional diagnostic methods often fail to detect Parkinson’s in its early stages, leading to delayed treatment and worsening of the disease’s impact on patients.
Current Diagnostic Challenges
Diagnosing Parkinson’s disease is a complex task that typically relies on clinical observations of symptoms, medical history evaluation, and neurological assessments.
However, due to the subtlety and variability of early-stage symptoms, misdiagnosis rates remain high, leading to delays in proper treatment and care.
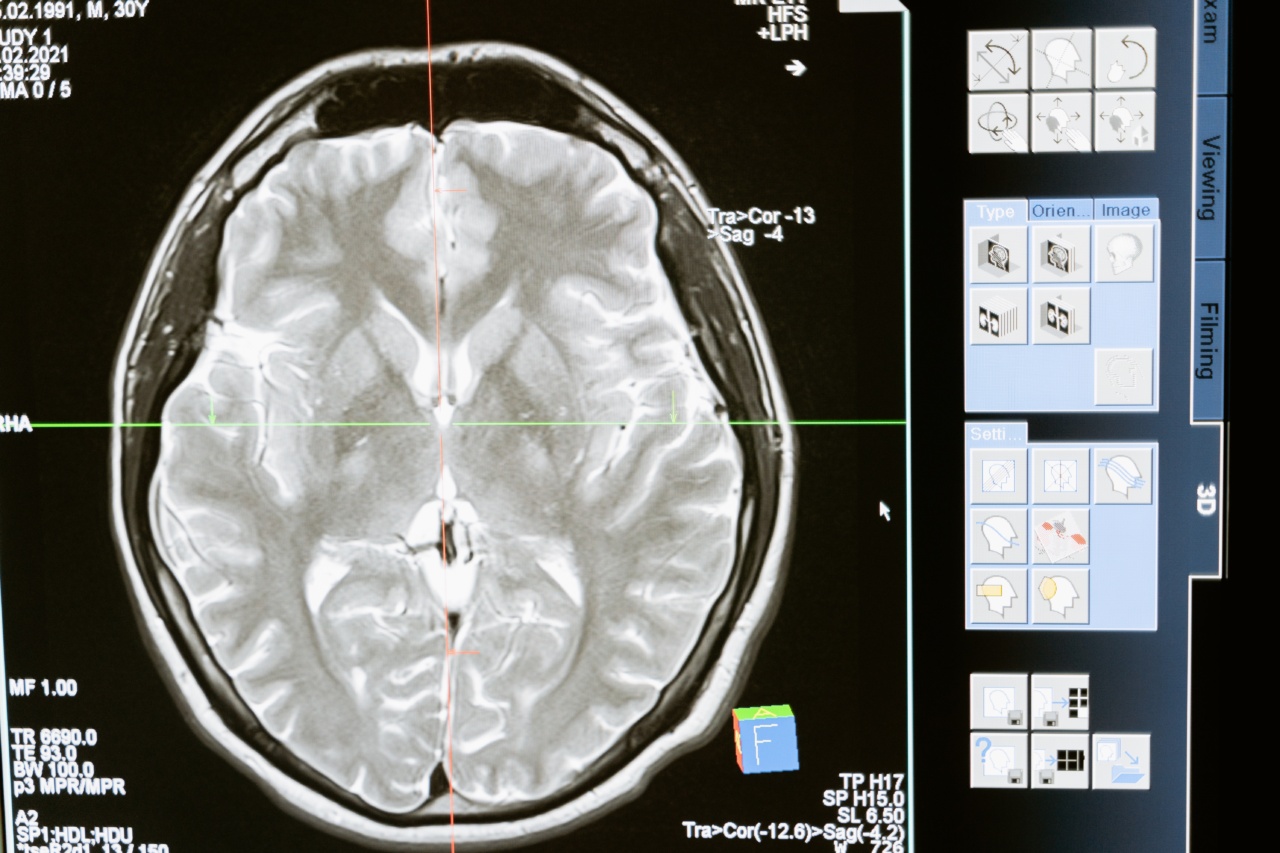
Furthermore, current diagnostic techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT) scans, lack the necessary sensitivity to detect the early signs of Parkinson’s disease.
These imaging methods primarily focus on structural changes and fail to capture the subtle functional alterations that occur in the brain, particularly during the disease’s early stages.
The Emergence of a Revolutionary Brain Scanning Method
In recent years, a groundbreaking brain scanning method has emerged as a potential game-changer in the early detection of Parkinson’s disease.
This innovative technique, known as Functional Magnetic Resonance Imaging (fMRI), has revolutionized the field of neuroscience and offers new hope for early and accurate Parkinson’s diagnosis.
Understanding Functional Magnetic Resonance Imaging (fMRI)
fMRI is an advanced imaging technique that measures and maps brain activity by detecting changes in blood flow and oxygenation.
Unlike traditional MRI, which focuses on anatomical structures, fMRI provides insights into the brain’s functional connectivity and activity patterns.
Using fMRI, researchers have discovered specific brain activity patterns associated with Parkinson’s disease.
By analyzing these patterns, they can identify early manifestations of the disease and distinguish them from other neurological conditions with similar symptoms.
Identifying Parkinson’s Disease Biomarkers
fMRI studies have shown that individuals with Parkinson’s disease exhibit distinct brain activity patterns compared to healthy individuals or those with other neurodegenerative disorders.
These unique patterns, known as biomarkers, are essentially neurological signatures that indicate the presence of Parkinson’s disease.
By developing algorithms that leverage these biomarkers, researchers can train machine learning models to accurately and efficiently identify individuals at risk of developing Parkinson’s or those in the early stages of the disease.
This groundbreaking approach opens up new possibilities for targeted interventions and personalized treatment plans.
The Advantages of Early Parkinson’s Detection
Early detection of Parkinson’s disease is critical for various reasons:.
1. Timely Treatment:
Early identification allows for the prompt initiation of appropriate treatment strategies.
Although there is currently no cure for Parkinson’s, several medications and therapies can help manage symptoms and slow down the progression of the disease, improving patients’ quality of life.
2. Disease Progression Monitoring:
Early detection enables healthcare professionals to closely monitor the disease’s progression, making adjustments to treatment plans as necessary.
By actively managing the disease from its initial stages, patients may experience improved overall outcomes and fewer complications.
3. Research Opportunities:
Identifying individuals in the early stages of Parkinson’s offers researchers the opportunity to study the disease’s progression and potentially develop novel therapeutic approaches.
Early detection plays a crucial role in advancing our understanding of Parkinson’s and accelerating the development of more effective treatments.
The Future of Parkinson’s Disease Diagnosis
The emergence of fMRI as a reliable and non-invasive method for early Parkinson’s detection holds immense promise for the future.
As researchers continue to refine their understanding of the disease’s biomarkers, the accuracy and accessibility of fMRI-based diagnostic approaches are expected to improve further.
Additionally, ongoing advancements in machine learning and artificial intelligence algorithms will enhance the efficiency and reliability of fMRI data analysis, enabling faster and more precise diagnoses.
These developments pave the way for early intervention strategies that can significantly improve patients’ lives.
Conclusion
The development of a revolutionary brain scanning method using fMRI represents a major breakthrough in the early detection of Parkinson’s disease.
By identifying unique biomarkers and leveraging the power of machine learning, researchers can now detect Parkinson’s at its earliest stages with a high degree of accuracy.
Early detection plays a crucial role in facilitating timely treatment, monitoring disease progression, and advancing research opportunities.
As fMRI technology continues to evolve and refine diagnostic approaches, there is newfound hope for improved patient outcomes and a brighter future for individuals living with Parkinson’s disease.