Diabetes, obesity, and cancer have become serious public health concerns in recent years, affecting millions of people worldwide. While these conditions are often considered separate entities, research has shown a significant link between them.
Studies have indicated that diabetes and obesity increase the risk of developing certain types of cancer, highlighting the need for further investigation and a multidimensional approach to tackle these health issues. Moreover, a groundbreaking study suggests that diabetes and obesity contribute to approximately 6% of cancer cases globally, shedding light on the magnitude of this interconnectedness.
The Diabetes and Obesity Epidemics
In the past few decades, the prevalence of diabetes and obesity has reached alarming levels.
According to the World Health Organization (WHO), nearly 422 million people worldwide are affected by diabetes, with approximately 1.6 million deaths directly attributed to the disease each year. Obesity, on the other hand, affects over 650 million adults worldwide, and its prevalence has tripled since 1975.
Both diabetes and obesity are complex and chronic conditions, with various causes and risk factors.
While genetic and environmental factors play a role, lifestyle choices such as poor diet, sedentary behavior, and lack of physical activity are key contributors to the development of these conditions. Additionally, obesity is a significant risk factor for the development of type 2 diabetes, further deepening the association between the two.
The Diabetes-Cancer Connection
Multiple studies have established a strong correlation between diabetes and an increased risk of certain types of cancer.
Individuals with diabetes have shown a higher likelihood of developing cancers such as liver, pancreas, colorectal, breast, bladder, and endometrial cancer. The underlying mechanisms for this association are still being explored, but researchers have proposed several hypotheses.
One theory suggests that high levels of insulin and insulin-like growth factor-1 (IGF-1), which are common in individuals with diabetes, may promote tumor growth.
Insulin resistance, a hallmark of type 2 diabetes, leads to increased insulin production to compensate for reduced cellular responsiveness. Elevated insulin levels can stimulate cancer cells to divide and grow, thereby increasing the risk of tumor formation.
Insulin and IGF-1 may also influence cancer progression by affecting other metabolic pathways.
These hormones can activate signaling pathways associated with cell proliferation, survival, and angiogenesis, all of which are crucial for tumor growth and development.
Inflammation is another factor that may contribute to the diabetes-cancer link. Chronic inflammation, often present in individuals with diabetes, can create an environment favorable for tumor formation and progression.
Inflammatory mediators, such as cytokines, growth factors, and chemokines, promote cell proliferation and survival, fostering an ideal setting for cancer cells.
Moreover, shared risk factors such as obesity and physical inactivity may explain the connection. Adipose tissue, particularly visceral fat, produces hormones and cytokines that can influence the development and progression of cancer.
Additionally, obesity-related inflammation, insulin resistance, and changes in hormone levels may collectively contribute to cancer development.
The Obesity-Cancer Connection
Similar to diabetes, obesity has been linked to an increased risk of several types of cancer. A meta-analysis of studies conducted worldwide estimated that excess body weight is responsible for approximately 3.6% of all cancer cases.
The link between obesity and cancer is believed to depend on various factors, including hormonal, metabolic, and inflammatory changes.
Adipose tissue, also known as fat tissue, produces hormones called adipokines, which can affect cell growth, inflammation, and insulin sensitivity.
An excessive accumulation of fat can alter the production and secretion of these hormones, leading to an imbalance that favors cancer development and progression.
Hormones such as estrogen, which is produced in adipose tissue, may also play a role in the obesity-cancer connection.
Elevated estrogen levels, a common occurrence in obese individuals, can increase the risk of developing hormone-related cancers, such as breast and endometrial cancer.
Furthermore, chronic low-grade inflammation associated with obesity can create a microenvironment that promotes cancer.
Adipose tissue produces pro-inflammatory cytokines that can stimulate cell proliferation and survival, contributing to the formation and spread of tumors.
The 6% Contribution
A comprehensive study published in The Lancet Oncology estimated that diabetes and obesity combined contribute to around 6% of all cancer cases worldwide.
This suggests that a significant proportion of cancer cases can be attributed to these two interconnected conditions, highlighting the urgency to address this health burden.
The study analyzed data from 12 types of cancer and found that the proportion of cancer cases attributable to diabetes and high body mass index (BMI) varies by cancer type.
Liver cancer had the highest contribution, with 38.4% of cases being linked to diabetes and high BMI. Endometrial cancer followed closely, with 33.7% of cases being attributed to these conditions.
The findings emphasize the need for preventive strategies that target diabetes and obesity in order to reduce the global cancer burden.
Implementing interventions aimed at reducing the prevalence of these conditions, such as promoting healthy eating habits, regular physical activity, and weight management, may contribute to a decrease in cancer incidence and mortality.
Multidimensional Approach for Prevention and Management
Given the intricate relationship between diabetes, obesity, and cancer, a multidimensional approach is crucial for prevention and management.
This approach should focus not only on individual-level interventions but also on societal, environmental, and policy changes.
Primary prevention efforts should aim at reducing the risk factors associated with diabetes, obesity, and cancer.
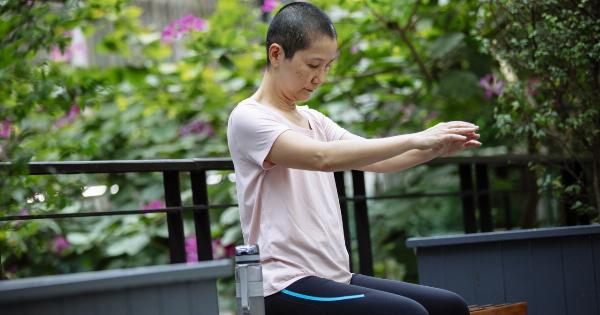
Encouraging healthy lifestyle habits, implementing comprehensive obesity prevention programs, and promoting early diabetes detection can play a significant role in preventing the development of cancer.
In addition, cancer screening and early detection programs, particularly in high-risk populations such as individuals with diabetes and obesity, can facilitate timely diagnosis and treatment.
Regular check-ups and screenings can help identify cancer at earlier stages when treatment options are more effective.
Furthermore, healthcare providers should adopt a holistic approach when managing individuals with diabetes or obesity. Addressing both conditions simultaneously can potentially improve health outcomes and reduce the risk of cancer development.
Integrating medical, dietary, and physical activity interventions can be highly beneficial for these individuals.
Conclusion
The link between diabetes, obesity, and cancer is undeniable. Research has shown a significant association between these conditions, with diabetes and obesity contributing to approximately 6% of global cancer cases.
Understanding the mechanisms behind this interconnectedness is crucial for developing effective preventive and management strategies.
Addressing the risk factors associated with diabetes and obesity through lifestyle modifications, early detection, and timely intervention can have a profound impact on reducing the burden of these chronic conditions and their associated cancers.
Through a multidimensional approach, individuals, healthcare professionals, and policymakers can work together to create a healthier future and diminish the impact of diabetes, obesity, and cancer on society.