Cancer is one of the leading causes of death worldwide. Despite significant advances in understanding the biology of cancer and development of novel therapeutic options, cancer remains a formidable health challenge.
One of the complications of cancer, particularly in advanced stages, is the development of cachexia, a condition marked by severe weight loss and muscle wasting. One of the biological factors contributing to cachexia is allocratic load. In this article, we explore the concept of allocratic load and its connection with cancer fatality.
What is Allocratic Load?
Allocratic load refers to the cumulative negative effects of chronic psychological, physiological, and environmental stressors.
These stressors impact several organ systems, including the immune, endocrine, and nervous systems, creating a state of chronic inflammation. The presence of chronic inflammation is associated with several health complications, including cardiovascular disease, neurodegenerative diseases, and cancer.
How is Allocratic Load Associated with Cancer?
Several studies have demonstrated a link between allocratic load and cancer development and progression.
Chronic inflammation, a hallmark of allocratic load, can contribute to cancer by enhancing the survival and proliferation of cancer cells and promoting angiogenesis. The inflammatory cells produce cytokines and chemokines, factors that can stimulate cancer cell growth and migration.
In addition, inflammation can promote immune system dysfunction, reducing the immune system’s ability to recognize and eliminate cancer cells.
Allocratic Load and Cachexia in Cancer
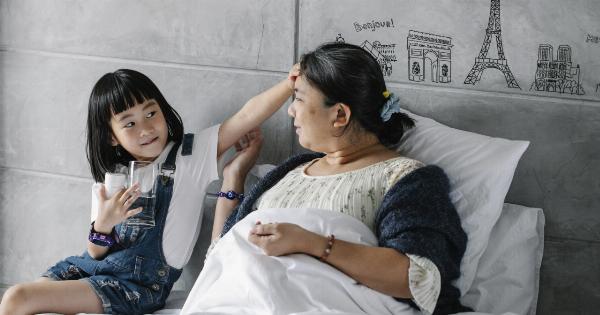
A significant complication of cancer, particularly in advanced stages, is the loss of body weight and muscle mass, a condition known as cachexia. Cachexia can contribute to poor quality of life and increased morbidity and mortality in cancer patients.
Allocratic load is thought to play a significant role in cachexia development in cancer patients. Chronic inflammation, a hallmark of allocratic load, can promote muscle wasting and induce changes in energy metabolism, resulting in weight loss.
In addition, the physical and emotional stress associated with cancer can contribute to allocratic load, exacerbating cachexia.
Measuring Allocratic Load in Cancer Patients
Several approaches have been developed to measure allocratic load in cancer patients. One of the commonly used markers is C-reactive protein (CRP), a protein produced by the liver in response to inflammation.
Elevated levels of CRP are associated with chronic inflammation and have been linked to poor cancer outcomes, including cachexia. Other markers of systemic inflammation, such as cytokines and chemokines, have also been studied as potential indicators of allocratic load in cancer patients.
Strategies to Reduce Allocratic Load in Cancer Patients
Given the significant impact of allostatic load on cancer outcomes, several strategies have been explored to reduce its impact on cancer patients.
Nutritional interventions, such as high-protein diets and omega-3 fatty acid supplementation, have been demonstrated to reduce inflammation in cancer patients and improve muscle mass. Exercise training has also been shown to improve inflammation markers and muscle mass in cancer patients.
In addition, psychological interventions, such as stress management and mindfulness-based therapies, have shown a positive impact on inflammation markers and quality of life of cancer patients.
Conclusion
Allocratic load, the cumulative negative effects of chronic psychological, physiological, and environmental stressors, is associated with several health complications, including cancer development and progression.
It plays a significant role in the development of cachexia, a complication of cancer marked by severe weight loss and muscle wasting. Measuring allocratic load in cancer patients can provide valuable insights into cancer outcomes and identify patients who may benefit from interventions to reduce stress and inflammation.
Strategies to reduce allocratic load, such as exercise training, nutritional interventions, and psychological therapies, have demonstrated positive effects on cancer outcomes and quality of life in cancer patients.