Stroke is one of the leading causes of death and disability worldwide. It occurs when the blood supply to the brain is disrupted, either due to a blockage or the rupture of a blood vessel.
The lack of oxygen and nutrients can cause irreversible damage to brain cells, leading to long-term impairments in speech, movement, and cognition. While there are treatments available to minimize the damage caused by a stroke, prevention remains the best approach.
The Role of Inflammation in Stroke
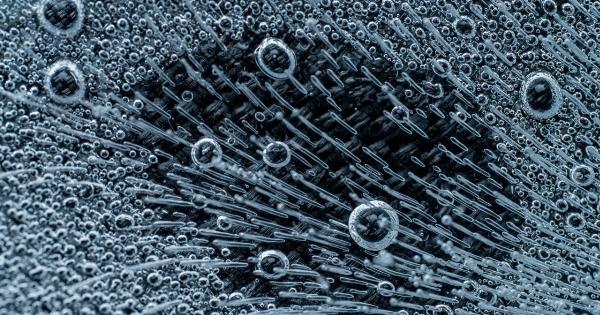
In recent years, researchers have been exploring the role of inflammation in stroke. Inflammation is the body’s immune response to injury or infection, and it involves the activation of various immune cells, including white blood cells.
While inflammation is crucial for the body to fight off infections and heal injuries, it can become harmful when it becomes chronic or excessive.
When a stroke occurs, inflammation is triggered in the affected area of the brain. This inflammatory response involves the recruitment of white blood cells, specifically a type of immune cell called leukocytes.
These white blood cells are responsible for defending the body against foreign invaders, but their role in stroke goes beyond that.
White Blood Cells as Double-Edged Swords
White blood cells play a dual role in stroke: they can either contribute to brain damage or promote healing. The outcome depends on the type of white blood cell involved and the stage of inflammation.
Neutrophils: The First Responders
Neutrophils are the first type of white blood cells to arrive at the site of a brain injury, including a stroke. They are highly efficient in eliminating pathogens and clearing cellular debris.
However, their powerful defense mechanisms can also cause collateral damage to healthy brain tissue. Neutrophils release harmful substances, such as reactive oxygen species and enzymes, which can lead to further brain injury.
Studies have suggested that limiting the activity of neutrophils in the early stages of stroke might be beneficial in reducing initial brain damage.
This can be achieved by blocking the migration of neutrophils into the brain or inhibiting their harmful substances. Preliminary animal studies have shown promising results in reducing infarct size and improving neurological outcomes.
Monocytes and Macrophages: The Clean-Up Crew
After the initial response by neutrophils, other white blood cells, such as monocytes and macrophages, come into play.
These cells are responsible for phagocytosing (engulfing) cellular debris and dead cells, thus promoting tissue repair and regeneration.
Monocytes are circulating immune cells that can differentiate into macrophages once they enter the brain. Macrophages have a critical role in clearing the damaged tissue and releasing factors that stimulate the healing process.
However, excessive or prolonged activation of macrophages can also contribute to tissue damage.
Research has been focused on understanding the mechanisms that control the transition between the damaging and protective roles of these white blood cells.
By regulating the activity of monocytes and macrophages, it might be possible to enhance their beneficial effects while suppressing their harmful actions.
T Cells: Linking Inflammation and the Brain
T cells, another type of white blood cell, have been found to play a crucial role in the interaction between the immune system and the brain. T cells are specialized immune cells that help regulate immune responses and maintain immune tolerance.
Studies have shown that activation of T cells occurs in stroke and can contribute to brain damage. These T cells release pro-inflammatory substances that can further exacerbate the inflammation and neuronal injury.
However, recent evidence suggests that certain types of T cells, known as regulatory T cells, have a protective role in stroke. These cells can suppress the inflammatory response and promote tissue repair, offering a potential target for therapeutic interventions.
Targeting White Blood Cells for Stroke Prevention
Based on the research conducted so far, targeting white blood cells offers a promising approach for stroke prevention. By modulating the activity of these cells, it might be possible to minimize brain damage and improve patient outcomes.
Several strategies are being explored to achieve this goal:.
1. Anti-inflammatory Drugs
Anti-inflammatory drugs could be used to reduce the excessive inflammatory response that occurs in stroke. By targeting specific molecules or pathways involved in the activation of white blood cells, these drugs could potentially limit brain damage.
However, caution must be exercised, as inflammation is essential for tissue repair, and excessive suppression could hinder the healing process.
2. Immune Cell Depletion
Another strategy is to deplete specific subsets of white blood cells, such as neutrophils or T cells.
This can be achieved by using antibodies or small molecules that specifically target these cells, preventing their migration or neutralizing their harmful substances. However, careful consideration must be given to the potential side effects of depleting vital immune cells, as they play essential roles in other aspects of the immune response.
3. Immunomodulation
Immunomodulatory approaches aim to modulate the immune response rather than completely suppressing it.
This could involve promoting the beneficial effects of certain white blood cells, such as monocytes and macrophages, while inhibiting the detrimental actions of others, like neutrophils and T cells. By striking the right balance, it might be possible to harness the protective mechanisms of the immune system while minimizing tissue damage.
Conclusion
White blood cells, particularly neutrophils, monocytes/macrophages, and T cells, play critical roles in the inflammation that occurs during a stroke.
Although their actions can both exacerbate and promote brain damage, targeting these immune cells offers a potential avenue for stroke prevention. Further research is needed to fully understand the complex interactions between white blood cells and the brain in stroke.
Ultimately, the hope is that by modulating the immune response, we can reduce the incidence and severity of strokes, leading to better outcomes for stroke patients.