Heart disease is a prevalent and concerning health issue, affecting millions of individuals worldwide. It is a leading cause of death and disability, making it crucial to understand the various factors that contribute to its development.
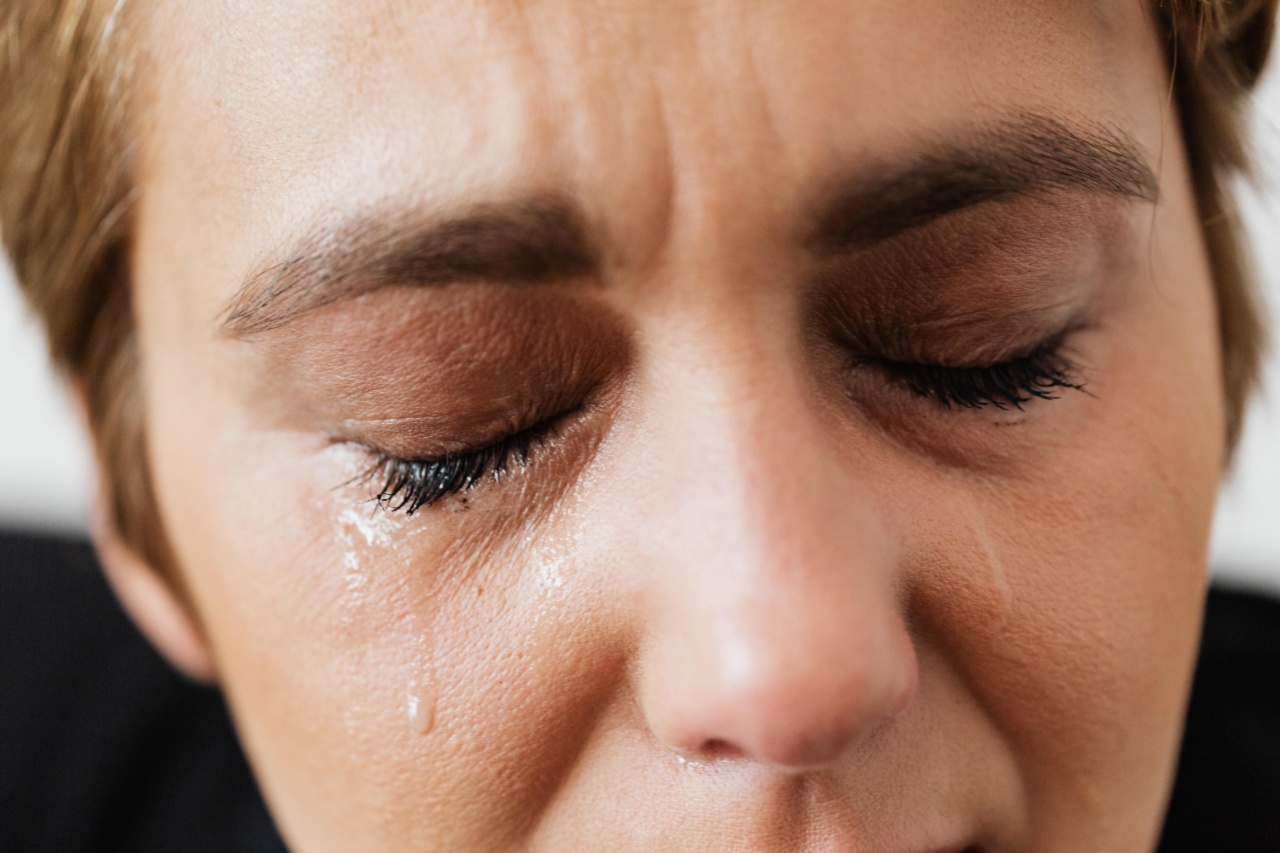
While factors such as smoking, poor diet, and lack of exercise are well-known risk factors, there is growing evidence linking mental health disorders, specifically depression, to an increased risk of heart disease. This article explores the role of depression in heart disease and highlights the importance of addressing mental health in cardiovascular care.
The Relationship Between Depression and Heart Disease
Depression is a common mental health disorder characterized by persistent feelings of sadness, loss of interest or pleasure, fatigue, and impaired concentration.
It affects approximately 300 million people worldwide, making it a significant global health concern. Studies have consistently shown that individuals with depression are more likely to develop heart disease compared to those without depression.
One of the mechanisms linking depression to heart disease is the influence of depression on various cardiovascular risk factors.
For instance, depression is associated with unhealthy behaviors such as smoking, physical inactivity, and poor dietary choices. These behaviors contribute to the development of risk factors like obesity, high blood pressure, and dyslipidemia, all of which increase the likelihood of developing heart disease.
Moreover, depression has been linked to physiological changes in the body, including increased inflammation and sympathetic nervous system activity.
Chronic inflammation is a key driver in the development and progression of atherosclerosis, a condition characterized by the buildup of plaque in the arteries, eventually leading to heart disease. Additionally, heightened sympathetic nervous system activity can increase blood pressure and heart rate, placing additional strain on the cardiovascular system.
Depression, Stress, and Heart Disease
Stress is an inevitable part of life, and while it is a natural response to challenging situations, excessive or prolonged stress can have detrimental effects on both mental and physical health.
Chronic stress is closely related to the development of depression and has been shown to contribute to the development of heart disease.
In individuals with depression, the body’s stress response becomes dysregulated, resulting in heightened and prolonged physiological stress reactions.
This chronic activation of the stress response system, characterized by elevated levels of stress hormones like cortisol, can lead to sustained increases in blood pressure, inflammation, and oxidative stress. These, in turn, contribute to the formation of atherosclerotic plaques and the progression of heart disease.
Furthermore, depression and chronic stress can affect behaviors that impact heart health.
Many individuals with depression experience a loss of motivation and energy, leading to reduced physical activity levels, neglect of self-care, and poor adherence to medication regimens. Additionally, some individuals turn to unhealthy coping mechanisms such as smoking, excessive alcohol consumption, or overeating, which can further exacerbate the risk of heart disease.
The Importance of Addressing Depression in Cardiovascular Care
Given the strong association between depression and heart disease, it is crucial for healthcare providers to recognize and address mental health concerns in individuals with cardiovascular disease.
Unfortunately, depression often goes undiagnosed and untreated in this population, leading to suboptimal health outcomes.
Integrating mental health screening and treatment into routine cardiovascular care can significantly improve patient outcomes.
Identifying and addressing depression early allows for appropriate management strategies to be implemented, which may include psychotherapy, medication, lifestyle modifications, and social support interventions.
Moreover, it is essential to emphasize a multidisciplinary approach to cardiovascular care, involving collaboration between cardiologists, general practitioners, psychiatrists, and other healthcare professionals.
By fostering an integrated approach, patients are provided with comprehensive care that addresses both their cardiovascular and mental health needs.
Reducing the Risk of Heart Disease: Strategies for Individuals with Depression
Individuals with depression and those at risk of heart disease can take several proactive steps to protect their cardiovascular health:.
1. Seek Professional Help
If you experience symptoms of depression, it is crucial to consult with a healthcare professional. They can provide an accurate diagnosis and recommend appropriate treatment options.
2. Participate in Psychotherapy
Talking therapies such as cognitive-behavioral therapy (CBT) and interpersonal therapy have been shown to be effective in treating depression.
Psychotherapy can equip individuals with coping mechanisms, stress management strategies, and a better understanding of their condition.
3. Engage in Regular Physical Activity
Exercise has been proven to have profound positive effects on mental health. Engaging in regular aerobic exercise, such as brisk walking or swimming, can help alleviate symptoms of depression while improving cardiovascular health.
4. Eat a Heart-Healthy Diet
Avoiding processed foods, reducing salt intake, and consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can significantly lower the risk of heart disease.
Additionally, certain nutrients, such as omega-3 fatty acids found in fatty fish, have been shown to promote mental well-being.
5. Practice Stress Reduction Techniques
Stress management techniques, such as mindfulness meditation, deep breathing exercises, and yoga, can help individuals with depression reduce stress levels and improve overall well-being.
Conclusion
Depression plays a significant role in the development and progression of heart disease. The relationship between depression, stress, and cardiovascular health is complex, involving behavioral, physiological, and psychological factors.
Recognizing and addressing depression in individuals with heart disease is crucial to improve overall health outcomes. By integrating mental health care into cardiovascular care, we can ensure that individuals receive comprehensive treatment that addresses both their physical and emotional well-being.