When it comes to healthcare, adhering to the advice and instructions provided by your doctor is crucial for your well-being. However, studies have shown that a significant number of patients do not fully comply with their doctors’ recommendations.
This nonadherence can have serious consequences on an individual’s health outcomes. To address this issue, researchers have been exploring innovative methods to determine whether patients are actively listening to their doctors.
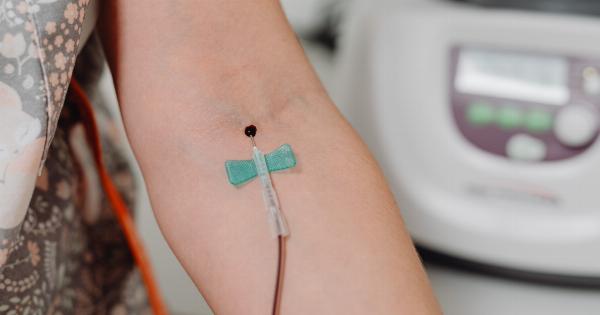
One groundbreaking approach involves the use of blood tests to analyze biomarkers that can indicate patient compliance. This article delves into the exciting research that suggests a blood test may provide insights into whether or not individuals are following their doctor’s advice.
The Challenge of Patient Nonadherence
Nonadherence to medical treatment recommendations is a widespread and persistent problem across the globe.
Several factors contribute to this issue, including forgetfulness, complex medication regimens, cost-related barriers, fear of side effects, and lack of understanding regarding the importance of treatment adherence.
When patients fail to follow their doctor’s advice, the effectiveness of their treatment may be compromised, leading to suboptimal health outcomes and increased healthcare costs.
This can be particularly problematic for individuals managing chronic conditions, where adherence to treatment plans plays a pivotal role in maintaining stable health.
Blood-Based Biomarkers and Adherence
Recent advancements in medical research suggest that blood tests may be able to provide valuable insights into a patient’s adherence to their prescribed treatment plan.
By examining specific biomarkers in the blood, researchers can identify indications of medication presence or changes in relevant biochemical levels that reflect adherence or nonadherence to treatment.
While blood tests have traditionally been used to diagnose diseases and monitor overall health, their potential application in assessing patient compliance is a relatively new area of investigation.
The identification of reliable biomarkers associated with medication use or other aspects of treatment adherence could revolutionize patient care and enable healthcare professionals to intervene promptly when nonadherence is detected.
Identifying Biomarkers for Adherence
In recent studies, researchers have focused on identifying biomarkers that can serve as indicators of adherence. One approach involves analyzing specific drug metabolites present in the blood.
These metabolites are byproducts of the body’s metabolic processes and can provide insight into a patient’s medication utilization. By understanding how drug metabolites are processed and eliminated from the body, doctors can assess whether patients are taking their medication as prescribed.
Additionally, researchers are exploring other potential biomarkers that may be related to treatment nonadherence. For instance, inflammatory markers, such as C-reactive protein (CRP), have been found to be elevated in nonadherent patients.
It is believed that the presence of high levels of inflammatory markers may be linked to increased disease activity due to inadequate adherence to prescribed therapies.
Implementing Blood-Based Adherence Testing
The implementation of blood tests for assessing treatment adherence presents both benefits and challenges. On one hand, blood tests are noninvasive and widely available, making them a convenient tool for routine monitoring.
However, several factors need to be considered for the successful integration of blood-based adherence testing into clinical practice.
Firstly, a standardized protocol for biomarker analysis and interpretation needs to be established to ensure consistency across different healthcare settings.
Laboratories must be able to accurately measure the chosen biomarkers and establish reliable reference ranges indicative of adherence or nonadherence.
Additionally, healthcare professionals require adequate training to understand the results of blood tests and interpret them in the context of each patient’s specific circumstances.
It is crucial to avoid making assumptions solely based on biomarker levels and consider other factors that may influence the results, such as disease progression, drug interactions, or patient-specific variations.
The Potential Impact on Patient Care
The integration of blood-based adherence testing into clinical practice has the potential to significantly improve patient care.
By identifying nonadherent individuals early on, healthcare providers can intervene and address the underlying reasons for noncompliance. This may involve adjusting treatment plans, providing additional education and support, or exploring alternative therapeutic options.
Moreover, blood tests can help differentiate between patients whose poor health outcomes are rooted in nonadherence versus those who experience treatment resistance or other factors beyond their control.
This differentiation is critical for optimizing treatment strategies and ensuring that patients receive the most appropriate interventions for their unique needs.
Future Implications and Challenges
While blood tests offer promising potential for assessing treatment adherence, there are challenges to overcome before widespread implementation in clinical practice.
One significant hurdle is the cost-effectiveness of these tests, both for patients and healthcare systems. The affordability and accessibility of blood tests will play a pivotal role in their acceptance and integration into routine care.
Furthermore, research is ongoing to identify additional biomarkers that can provide more comprehensive insights into patient adherence.
A multidimensional approach, incorporating various biological molecules and factors, may offer a more accurate and nuanced understanding of adherence behaviors. Continued research and innovation in this field are crucial to refine blood-based adherence testing and optimize its clinical utility.
Raising Awareness and Empowering Patients
While blood tests may offer a valuable tool for assessing treatment adherence, it is important to approach this potential development with sensitivity and caution.
Patient autonomy and the doctor-patient relationship should be respected and preserved throughout this process. Medical professionals should continue to prioritize patient education and involvement in treatment decisions, empowering individuals to understand the importance of adherence and take an active role in managing their own health.
Conclusion
The integration of blood tests for assessing treatment adherence represents a promising development in healthcare.
By leveraging specific biomarkers, healthcare providers may gain objective insights into patient compliance, enabling them to optimize treatment strategies and improve health outcomes. While challenges remain, further research and innovation in this field have the potential to transform patient care and enhance the effectiveness of medical interventions.