Inflammatory bowel disease (IBD) is the term used to describe chronic inflammation of the digestive tract. It is a serious medical condition that affects millions of people worldwide.
IBD affects both men and women and can occur at any age, although it is most commonly diagnosed in the late teens to early 30s. The two most common forms of IBD are Crohn’s disease and ulcerative colitis.
What Causes Inflammatory Bowel Disease?
The exact cause of IBD is not known, but it is believed to be linked to an abnormal immune system response. There may also be a genetic component to IBD, as it tends to run in families.
Certain triggers may also cause flare-ups of IBD, including stress, infections, and certain foods.
How Does Inflammatory Bowel Disease Affect the Body?
IBD can cause a wide range of symptoms, including abdominal pain, diarrhea, cramping, and fatigue. Because IBD causes inflammation in the digestive tract, it can also cause damage to the lining of the intestines.
This can lead to complications such as malnutrition, anemia, and dehydration.
How Can Diet Help Manage Inflammation in Inflammatory Bowel Disease?
While there is no cure for IBD, certain lifestyle changes can help manage symptoms and prevent flare-ups. One of the most important lifestyle changes you can make is to focus on a healthy diet.
There is no one-size-fits-all diet for IBD, as each person’s body may react differently to different foods. However, there are certain guidelines that can be helpful for managing inflammation in IBD.
Eat a Balanced Diet
Eating a balanced diet is important for everyone, but even more so for those with IBD. A balanced diet includes a variety of foods from all food groups, including whole grains, fruits, vegetables, lean proteins, and healthy fats.
When choosing carbohydrates, opt for complex carbohydrates such as whole grains, fruits, and vegetables rather than simple carbohydrates like sugary foods and refined grains.
Avoid Trigger Foods
Some foods may trigger flare-ups in people with IBD. Specific trigger foods vary from person to person, but common trigger foods include:.
- Dairy products
- Fatty and fried foods
- Spicy foods
- Caffeine and alcohol
- High-fiber foods (such as beans and certain fruits and vegetables)
If you notice that certain foods trigger flare-ups, try to avoid those foods or limit them in your diet.
Choose Anti-Inflammatory Foods
Some foods have anti-inflammatory properties that can help manage inflammation in the body. Incorporating these foods into your diet may help manage IBD symptoms. Anti-inflammatory foods include:.
- Fatty fish, such as salmon and tuna
- Leafy greens, such as spinach and kale
- Berries, such as blueberries and strawberries
- Turmeric
- Ginger
- Beans and legumes
Adding these foods to your diet can help reduce inflammation in the body and manage IBD symptoms.
Consider a Low-FODMAP Diet
FODMAPs are certain types of carbohydrates that can be difficult to digest for some people. A low-FODMAP diet may be helpful for managing symptoms in those with IBD.
The low-FODMAP diet involves avoiding foods high in certain types of carbohydrates, including:.
- Fructose (found in some fruits and sweeteners)
- Lactose (found in dairy products)
- Fructans (found in wheat, onions, and garlic)
- Galactans (found in beans and legumes)
- Polyols (found in some fruits and sugar-free sweeteners)
If you are interested in trying the low-FODMAP diet, it’s important to work with a registered dietitian to ensure that you are getting all the nutrients you need.
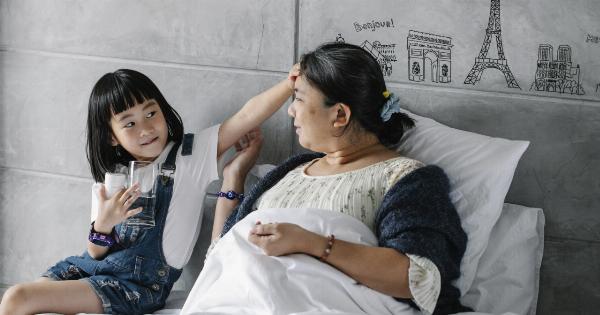
Stay Hydrated
Staying hydrated is important for everyone, but especially for those with IBD. Diarrhea and vomiting can cause dehydration, so it’s important to drink plenty of fluids.
Water is the best choice, but other hydrating beverages like herbal tea and coconut water can also be helpful. Avoid drinks with caffeine and alcohol, as they can further dehydrate the body.
Final Thoughts
Inflammatory bowel disease is a complex medical condition that requires a team approach for management. Along with medical treatment, lifestyle changes such as a healthy diet can help manage inflammation and prevent flare-ups.
Remember to work with your healthcare team to create a personalized diet plan that meets your individual needs.