Sex is a natural and healthy part of life, yet due to social taboos and cultural influences, it remains a topic that is often shrouded in myths and misconceptions.
Similarly, contraception, which plays a crucial role in preventing unintended pregnancies and promoting safe sexual practices, is clouded by misunderstandings that can hinder access and use. In this article, we aim to dispel some of the most common myths surrounding sex and contraception, fostering a better understanding of these essential aspects of reproductive health.
Myth 1: Only Promiscuous individuals need contraception.
This myth perpetuates the notion that those who engage in casual or multiple sexual relationships are the only ones at risk of unintended pregnancies or sexually transmitted infections (STIs).
In reality, individuals in committed monogamous relationships also need contraception as it helps them plan and space their desired pregnancies. Moreover, condoms and other barrier methods remain one of the most effective ways to prevent the transmission of STIs.
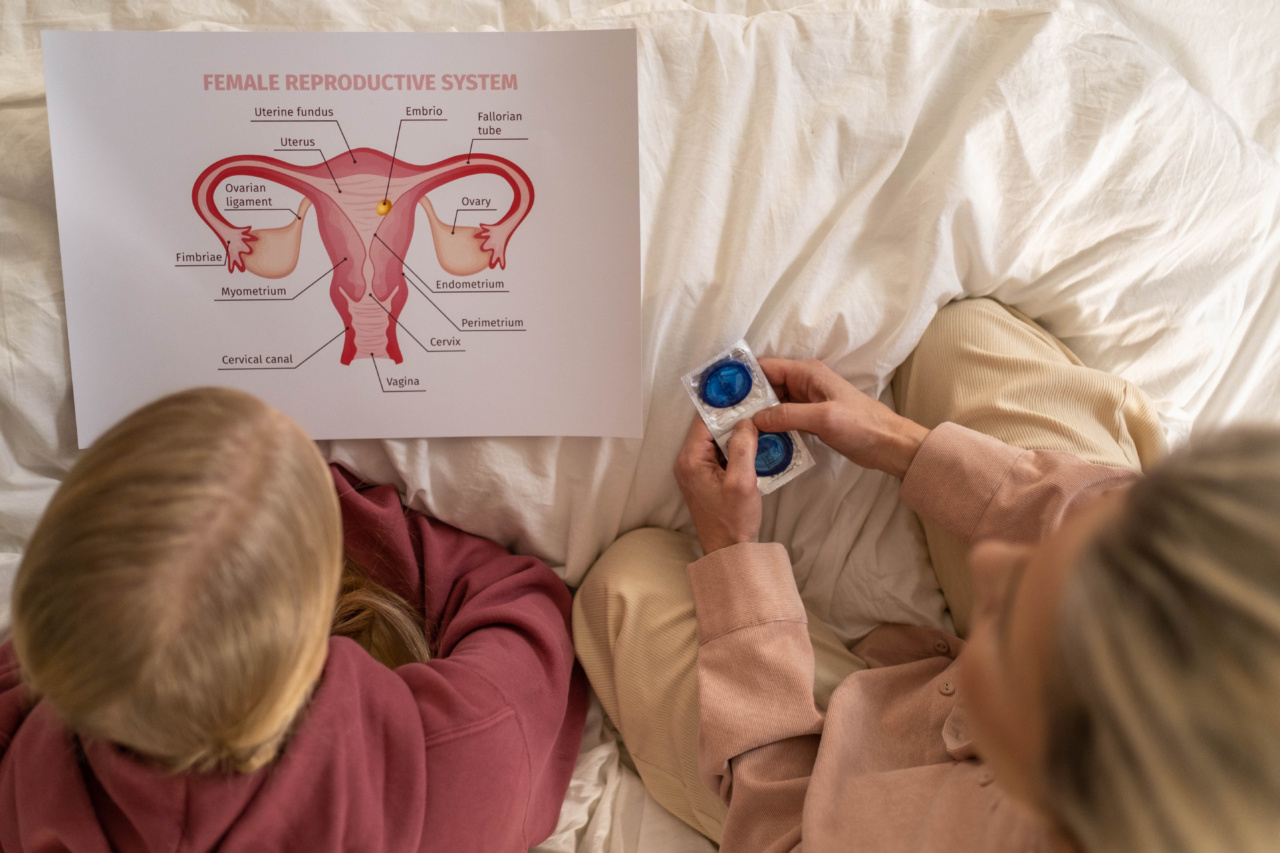
Myth 2: Contraception is solely a woman’s responsibility.
While women have more contraceptive options available to them, contraception is a shared responsibility between sexual partners.
Open communication, mutual understanding, and joint decision-making about contraception can help couples find the method that suits them best. Both men and women should actively participate in discussions and efforts to prevent unintended pregnancies and safeguard their sexual health.
Myth 3: All contraceptive methods are the same.
There is a wide variety of contraceptive methods available, each with its own set of advantages, disadvantages, and efficacy rates.
From hormonal methods like oral contraceptives or contraceptive patches to barrier methods such as male and female condoms, the choices are diverse. Additionally, long-acting reversible contraception (LARC), like intrauterine devices (IUDs) and implants, provides highly effective and reversible options.
Consulting a healthcare professional can help individuals and couples identify the most suitable contraceptive method for their needs and lifestyles.
Myth 4: Contraception causes infertility.
This myth is a significant barrier to contraceptive use, especially among women. Contraception does not cause infertility. After discontinuing most contraceptive methods, fertility rapidly returns to pre-use levels.
It is crucial to separate this misconception from the fact that certain sexually transmitted infections, if left untreated, can lead to infertility. Contraception, when used correctly, helps prevent unintended pregnancies without causing long-term reproductive issues.
Myth 5: The withdrawal method is an effective form of contraception.
The withdrawal method, also known as “pulling out,” involves the man withdrawing his penis from the vagina before ejaculation. While it may seem like a simple and accessible form of contraception, it is highly unreliable and ineffective.
It offers no protection against STIs and poses a significant risk of pregnancy due to the presence of sperm in pre-ejaculatory fluid. For reliable contraception, it is essential to use proven methods such as hormonal contraception, barrier methods, or LARC.
Myth 6: Emergency contraception is the same as abortion.
Emergency contraception, often referred to as the “morning-after pill,” is used to prevent pregnancy after unprotected sex or contraceptive failure. It works primarily by preventing or delaying ovulation.
Emergency contraception is not an abortifacient; it does not end a pregnancy or harm an embryo. It is crucial to have timely access to emergency contraception to prevent unintended pregnancies, especially in cases of rape or contraception mishaps.
Myth 7: Contraception leads to weight gain.
Weight gain is a concern often associated with hormonal methods of contraception, such as oral contraceptives or injectable hormonal methods.
While some individuals may experience slight weight changes, studies have shown that they are not clinically significant and are likely due to other factors. Weight gain is a complex issue influenced by various factors like lifestyle, genetics, and aging. Those concerned about weight changes can discuss alternative contraceptive methods or lifestyle modifications with healthcare professionals.
Myth 8: Using contraception means one is engaging in underage or immoral sexual behavior.
Contraception is not an endorsement or encouragement of underage or immoral sexual behavior. It is instead an important tool used by individuals who are sexually active and wish to prevent unintended pregnancies or protect themselves from STIs.
Accepting and supporting contraceptive use helps create a safe and non-judgmental environment for individuals, promoting responsible sexual behavior and reproductive health.
Myth 9: Contraception is only for women of a certain age.
While it is true that many women use contraception during their reproductive years, contraception is not limited to a specific age group. Contrary to popular belief, women in their 40s and perimenopausal stages can still become pregnant.
Contraception should be considered until menopause is confirmed, as unintended pregnancies can occur at any age. Consulting with a healthcare professional can help women select the appropriate method that aligns with their age and reproductive goals.
Myth 10: Natural or traditional methods of contraception are highly effective.
Traditional or natural contraceptive methods, such as tracking menstrual cycles (rhythm method) or monitoring basal body temperature, can be utilized for contraception, but they are less reliable than modern contraceptive methods.
Factors like irregular periods, changes in hormonal patterns, and external influences can affect the accuracy of these methods. While these methods can be used for contraception, it is essential to understand their limitations and consider combining them with other reliable methods or seeking professional guidance.