Compulsive disorders, also known as obsessive-compulsive disorders (OCD), are a type of mental illness characterized by recurrent, distressing, and intrusive thoughts (obsessions) and repetitive, ritualistic behaviors (compulsions).
These disorders can significantly impair an individual’s daily functioning and overall quality of life. While traditional treatments for OCD include medication and therapy, emerging research suggests that in-depth brain stimulation may hold promise in effectively treating compulsive disorders.
Understanding Compulsive Disorders
Compulsive disorders are complex conditions that can manifest in various ways. Some common types of OCD include:.
- Checking OCD: Individuals compulsively check or verify things repeatedly, such as locked doors or switched-off appliances.
- Cleaning OCD: People with cleaning OCD have an intense fear of contamination and engage in excessive cleaning rituals.
- Ordering OCD: This involves the need for things to be arranged in a particular order or symmetry, and any disruption of this order causes distress.
- Hoarding OCD: Individuals with hoarding OCD struggle to discard possessions and accumulate an overwhelming amount of items.
- Counting OCD: People with this form of OCD engage in repetitive counting or perform tasks a specific number of times, often to alleviate anxiety.
These are just a few examples, and OCD can manifest in numerous other ways, affecting different aspects of an individual’s life.
Treatment Options for Compulsive Disorders
Traditionally, a combination of psychotherapy (usually cognitive-behavioral therapy) and medication (such as selective serotonin reuptake inhibitors) has been the standard treatment for compulsive disorders.
Cognitive-behavioral therapy (CBT) focuses on helping individuals identify and change negative thought patterns and behaviors associated with OCD.
It involves exposure and response prevention (ERP), where patients are gradually exposed to situations that trigger their obsessions and learn to resist engaging in compulsions. CBT has been proven effective in treating OCD, but it may not work for everyone.
Medication, particularly selective serotonin reuptake inhibitors (SSRIs), is commonly prescribed to manage the symptoms of OCD. SSRIs help regulate serotonin levels in the brain, which is believed to be imbalanced in individuals with OCD.
While medication can alleviate symptoms, it is often not a standalone solution and is more effective when used in conjunction with therapy.
The Potential of In-Depth Brain Stimulation
Recent advancements in neuroscience have paved the way for exploring novel treatment options for compulsive disorders.
One such approach is in-depth brain stimulation, which involves directly targeting specific regions of the brain to modulate activity and alleviate symptoms.
Deep brain stimulation (DBS) is a technique that has shown promise in treating various neurological and psychiatric disorders, including Parkinson’s disease and major depression.
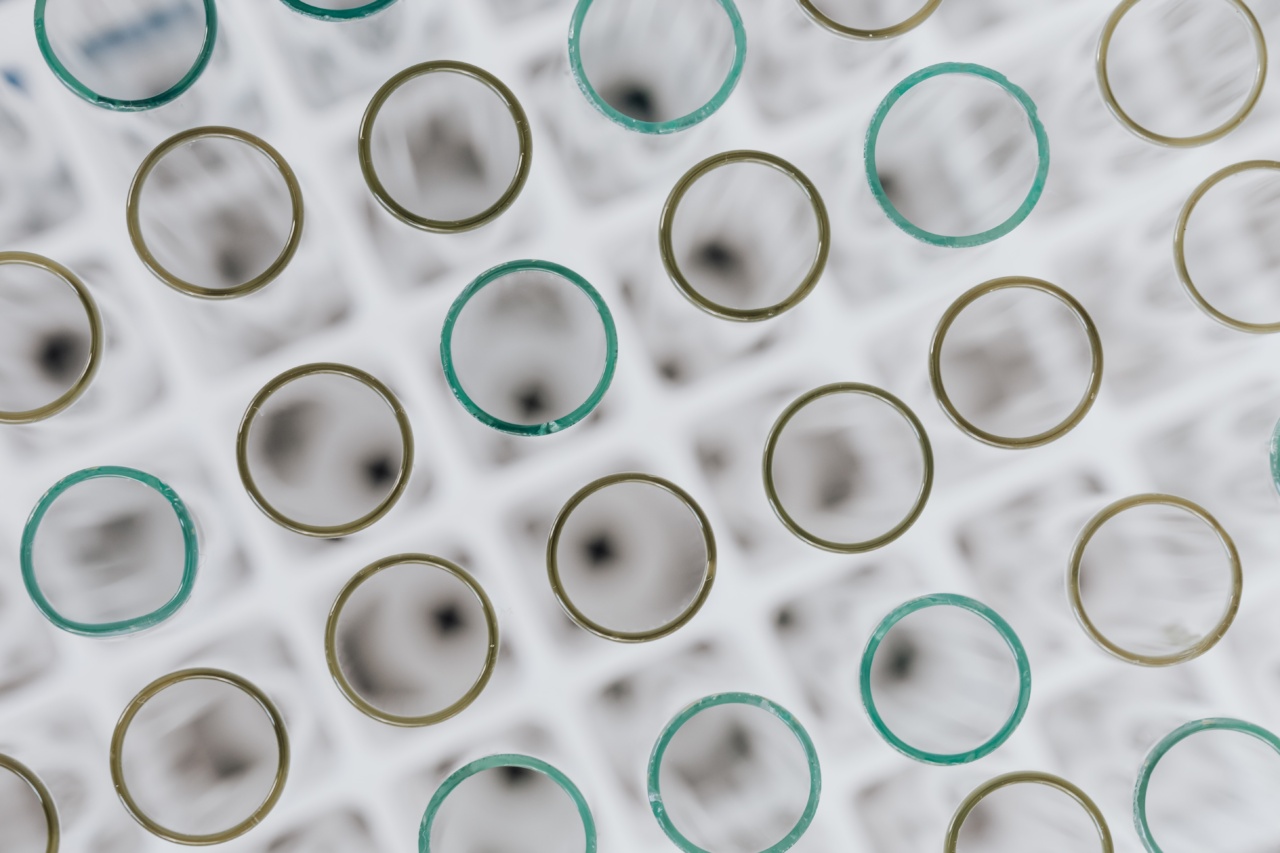
DBS involves implanting electrodes deep within the brain and delivering electrical impulses to specific regions.
Research now suggests that DBS may also be effective in treating compulsive disorders.
By targeting the cortico-striato-thalamo-cortical (CSTC) circuitry, which is implicated in OCD, DBS can potentially disrupt the abnormal neural activity contributing to obsessions and compulsions.
Studies Supporting the Efficacy of Deep Brain Stimulation
Several studies have provided evidence supporting the use of deep brain stimulation for the treatment of compulsive disorders.
In a landmark study published in JAMA Neurology, researchers conducted a randomized, double-blind trial involving individuals with severe, treatment-resistant OCD.
The study found that DBS targeting the ventral capsule/ventral striatum significantly reduced OCD symptoms compared to the control group who received sham stimulation.
Another study published in Biological Psychiatry explored the long-term effects of deep brain stimulation in patients with OCD. Participants experienced sustained improvement in their symptoms even five years after undergoing DBS.
Furthermore, a meta-analysis published in JAMA Psychiatry analyzed data from multiple studies and found that deep brain stimulation, specifically targeting the subthalamic nucleus and nucleus accumbens, led to significant reductions in OCD symptoms as measured by standardized rating scales.
Challenges and Limitations
While the results of these studies are promising, deep brain stimulation for compulsive disorders is not without challenges and limitations.
Firstly, the procedure itself is invasive and carries potential risks, including infection, bleeding, and cognitive side effects.
The precise placement of electrodes within delicate brain structures is crucial, and careful patient selection is warranted.
Additionally, the impact of deep brain stimulation on long-term neurocognitive function is still not fully understood. Further research is necessary to determine the potential cognitive effects and ensure the safety of this treatment modality.
Moreover, deep brain stimulation is currently not widely available and is primarily reserved for severe, treatment-resistant cases of OCD due to its invasiveness and the expertise required to administer the treatment.
Its high cost also poses a practical barrier to wider implementation.
The Future of Compulsive Disorder Treatment
In-depth brain stimulation, including deep brain stimulation, represents a promising avenue for the future treatment of compulsive disorders.
While further research is needed to optimize the technique, refine patient selection criteria, and establish long-term safety and efficacy profiles, the initial findings indicate significant potential.
Advancements in brain imaging technologies, such as functional magnetic resonance imaging (fMRI), can aid in identifying specific neural circuits involved in OCD, leading to more targeted stimulation approaches.
Non-invasive techniques like transcranial magnetic stimulation (TMS) are also being explored as potential alternatives to invasive deep brain stimulation.
With continued research and innovation, in-depth brain stimulation may revolutionize the way we approach compulsive disorders, offering hope to those who have not responded to traditional treatments.
Conclusion
Compulsive disorders are debilitating mental illnesses that can significantly impact an individual’s life.
While traditional treatments such as therapy and medication have shown efficacy, in-depth brain stimulation, particularly deep brain stimulation, holds promise as a novel and potentially transformative approach for treating compulsive disorders.
Research studies have demonstrated the effectiveness of deep brain stimulation in reducing OCD symptoms, providing hope for individuals who have not found relief through conventional methods.
However, challenges and limitations remain, including invasiveness, cost, and the need for further research to optimize the technique and ensure long-term safety.
The future of compulsive disorder treatment may lie in advancements in brain stimulation techniques and a deeper understanding of the neural circuitry underlying these disorders.
With continued research and innovation, in-depth brain stimulation may open new avenues for those living with the burden of compulsive disorders.