Septicemia, also known as sepsis, is a life-threatening condition that occurs when the body’s response to infection causes widespread inflammation.
It is a severe immune response to bacterial, fungal, or viral infections that spread to the bloodstream. This condition can lead to organ failure, septic shock, and even death if not treated promptly. To effectively understand and manage septicemia, it is essential to be aware of its causes, symptoms, risk factors, and treatment options.
Causes of Septicemia
Septicemia usually occurs when an infection that starts in a particular part of the body, such as the lungs, urinary tract, or skin, spreads to the bloodstream.
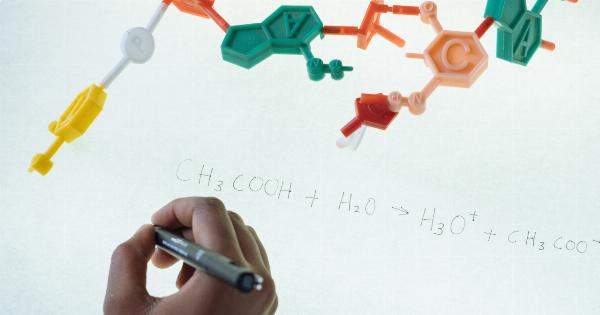
Common sources of infection include pneumonia, urinary tract infections, abdominal infections, and skin infections like cellulitis. Bacteria such as Escherichia coli (E. coli), Streptococcus, and Staphylococcus aureus are frequently involved in causing septicemia. Fungal and viral infections can also lead to septicemia, although they are less common causes.
Symptoms of Septicemia
Recognizing the symptoms of septicemia is crucial for early detection and intervention. The signs and symptoms can vary depending on the severity of the infection and the individual’s overall health. Common symptoms of septicemia include:.
1. Fever and chills: Persistent high fever and chills that do not improve with usual treatments may indicate septicemia.
2. Rapid heartbeat: An abnormally fast heart rate, known as tachycardia, is a typical sign of septicemia.
3. Rapid breathing: Increased respiratory rate or shortness of breath can be indicative of septicemia.
4. Confusion and altered mental status: In severe cases, septicemia can cause confusion, decreased alertness, and even unconsciousness.
5. Low blood pressure: A drop in blood pressure, known as hypotension, can occur as septicemia progresses, increasing the risk of septic shock.
6. Skin rash: A reddish or purplish rash that does not disappear when pressure is applied is a potential symptom of septicemia.
7. Fatigue and weakness: Feeling excessively tired and weak without a clear cause may indicate septicemia.
8. Decreased urine output: Severe infections can impair kidney function, leading to reduced urine production.
9. Gastrointestinal symptoms: Nausea, vomiting, and diarrhea can be associated with septicemia.
10. Pain and discomfort: The site of the initial infection or the entire body may experience pain and discomfort.
Risk Factors for Septicemia
While septicemia can affect anyone, certain factors increase the risk of developing this severe condition:.
1. Age: The very young and older adults are more susceptible to septicemia due to their weaker immune systems.
2. Chronic medical conditions: Individuals with chronic diseases such as diabetes, kidney disease, liver disease, HIV/AIDS, or cancer have a higher risk of septicemia.
3. Weakened immune system: People with weakened immune systems, whether due to underlying conditions or medications like immune-suppressing drugs, are more vulnerable to septicemia.
4. Hospitalization: Being in a healthcare facility, especially intensive care units, exposes individuals to potential healthcare-associated infections that can progress to septicemia.
5. Recent surgeries: Surgical procedures carry a risk of introducing infections, increasing the likelihood of septicemia.
6. Catheter use: Indwelling catheters, such as urinary or intravenous catheters, can serve as entry points for bacteria, leading to septicemia.
7. Immunization status: Not being up-to-date with vaccinations raises the risk of certain infections that can progress to septicemia.
8. Substance abuse: Alcohol or drug abuse weakens the immune system and exposes individuals to infections that can lead to septicemia.
9. Recent history of infections: People who recently had infections or are currently under treatment for an infection are at a higher risk of developing septicemia.
10. Frequent exposure to healthcare settings: Healthcare workers and individuals who visit healthcare facilities frequently have an increased risk of infection and subsequent septicemia.
Diagnosing Septicemia
The diagnosis of septicemia involves a combination of clinical evaluation, medical history review, and specific medical tests:.
1. Physical examination: The healthcare provider examines the patient’s vital signs, overall condition, and any visible signs of infection, such as inflammation or redness.
2. Blood cultures: Collecting blood samples to culture and identify the bacteria or microorganisms causing the infection is crucial in diagnosing septicemia and determining the appropriate treatment.
3. Complete blood count (CBC): This test analyzes the number and types of blood cells. A high white blood cell count, along with other specific indicators, can suggest an infection.
4. Blood chemistry tests: These tests assess various parameters of organ function, such as liver and kidney function, which may be affected by septicemia.
5. Imaging tests: X-rays, ultrasounds, CT scans, or MRIs may be conducted to identify any potential sources of infection, such as abscesses or pneumonia.
6. Urine and other fluid cultures: If a specific infection site is suspected, fluid samples may be collected for culture and identification of pathogens.
Treatment Options for Septicemia
Septicemia requires immediate medical attention and treatment in a hospital setting, typically in an intensive care unit.
The chosen treatment options depend on the severity of the infection, the likely causative organisms, and the patient’s overall health.
1. Intravenous antibiotics: Broad-spectrum antibiotics are administered promptly after blood cultures are obtained to cover a wide range of potential pathogens.
Once the specific bacteria or microorganism responsible for the infection are identified, the antibiotics may be adjusted accordingly.
2. Medications to stabilize blood pressure: In cases where septicemia leads to a drop in blood pressure, medications like vasopressors may be administered to maintain adequate blood flow to vital organs.
3. Supportive care: Patients with septicemia often require supportive treatments, such as oxygen therapy, intravenous fluids, and close monitoring of vital signs.
4. Source control: If the infection source, such as an abscess or infected catheter, is identified, it is crucial to remove or drain the source to eliminate the infection entirely.
5. Immune therapies: In some cases, medications that modulate the immune response, such as intravenous immunoglobulins or immunomodulatory drugs, may be considered as adjunctive treatments.
Preventing Septicemia
Prevention plays a crucial role in reducing the risk of septicemia and its complications:.
1. Practice proper hand hygiene: Regular handwashing with soap and warm water or using alcohol-based hand sanitizers helps prevent the spread of bacteria and viruses.
2. Keep wounds clean and protected: Clean any cuts, scrapes, or wounds promptly and cover them with sterile dressings to prevent infections.
3. Ensure up-to-date vaccinations: Stay current on recommended vaccines, such as those for influenza, pneumonia, and bacterial infections like meningococcus.
4. Follow safe injection practices: Ensure needles and syringes are sterile and used only once, and safely dispose of them in appropriate containers.
5. Maintain a healthy immune system: Eat a balanced diet, exercise regularly, manage stress, get enough sleep, and avoid risky behaviors to keep your immune system strong.
6. Be cautious in healthcare settings: If you are in a hospital or other healthcare facilities, follow infection control measures, such as proper hand hygiene, wearing masks, and adhering to sterile procedures.
7. Practice safe sex: Using barrier methods like condoms reduces the risk of sexually transmitted infections that can lead to septicemia.
Conclusion
Septicemia is a life-threatening condition that requires immediate medical attention. Understanding its causes, recognizing the symptoms, and knowing the risk factors can help in early detection and timely intervention.
With prompt treatment, proper antibiotic administration, and supportive care, the prognosis for septicemia has improved over the years. However, prevention remains crucial in reducing the incidence of septicemia. Practicing good hygiene, following safe healthcare practices, and maintaining a healthy immune system are essential in preventing this severe condition.