Parkinson’s disease is a degenerative disorder of the nervous system that affects movement. It is a progressive condition that primarily affects the motor system, causing symptoms such as tremors, stiffness, and slowness of movement.
While there is no cure for Parkinson’s disease, early diagnosis is crucial for managing symptoms and improving the quality of life for patients. Traditionally, Parkinson’s has been diagnosed based on clinical observation and subjective assessments.
However, recent research suggests that analyzing a person’s gait or walking pattern can help in the early detection of Parkinson’s disease.
The Link Between Parkinson’s and Gait
Walking is a complex motor task that involves the coordination of various body systems, including the musculoskeletal and nervous systems.
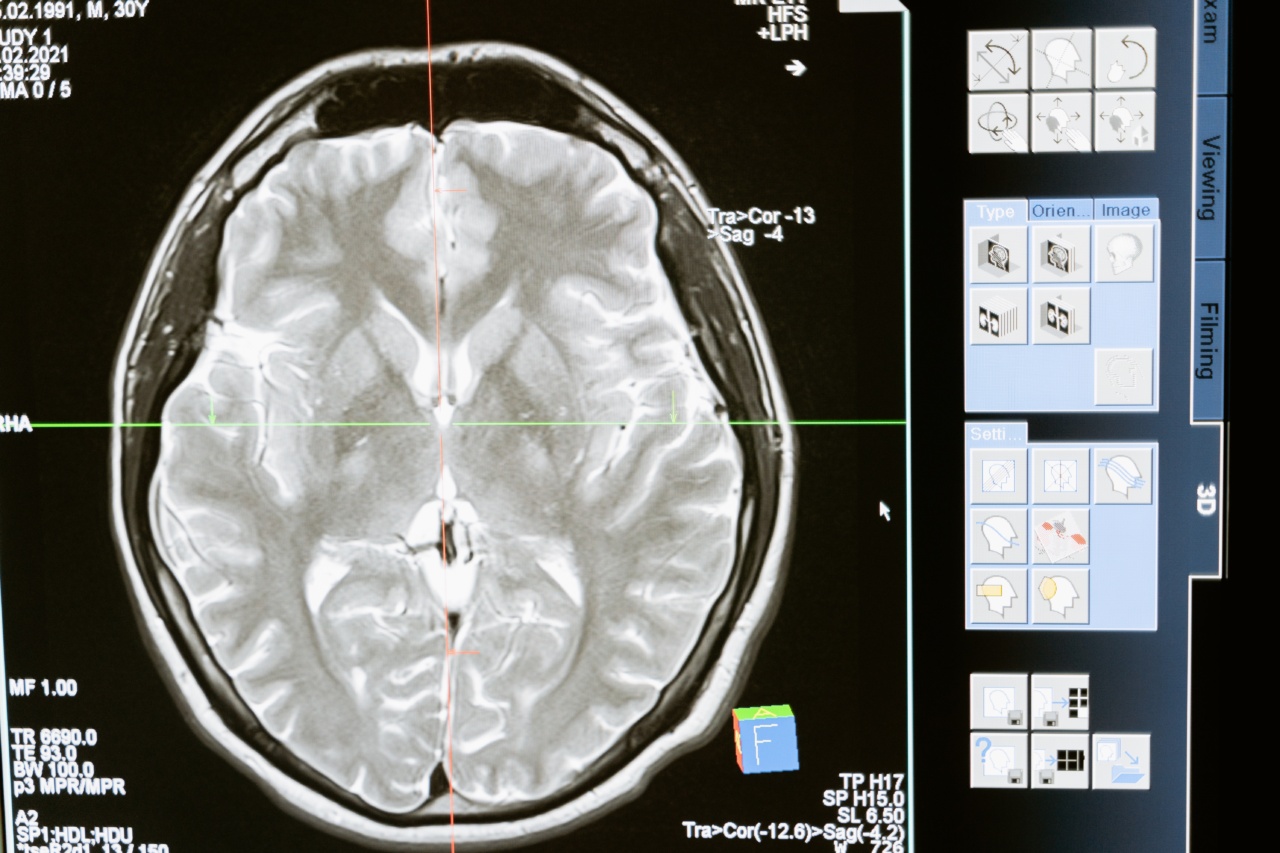
In Parkinson’s disease, the basal ganglia, a region of the brain responsible for controlling movement, gradually degenerates. This results in an impairment of the motor function and affects a person’s gait.
Studies have shown that people with Parkinson’s disease exhibit distinct changes in their gait compared to healthy individuals.
These changes include reduced step length, shuffling gait, reduced arm swing, and increased variability in step timing and stride length. Although these changes may be subtle in the early stages of the disease, an analysis of gait could provide valuable insights for early Parkinson’s diagnosis.
Advancements in Gait Analysis Technology
Thanks to advancements in technology, gait analysis has become more accessible and reliable for early Parkinson’s diagnosis.
Researchers have developed wearable devices, such as accelerometers and gyroscopes, that can be attached to the body to measure and quantify gait parameters.
Accelerometers, for example, can detect body movement and measure various gait parameters, including step length, stride length, cadence, and walking speed.
By comparing these measurements to established normative data, healthcare professionals can identify deviations from the expected gait pattern and potentially diagnose Parkinson’s disease at an early stage.
Additionally, smartphone applications have also been developed that utilize the built-in sensors, such as accelerometers and gyroscopes, to analyze a person’s gait.
These apps provide a convenient and cost-effective way to collect gait data, making early Parkinson’s diagnosis more accessible.
The Role of Artificial Intelligence in Gait Analysis
Artificial intelligence (AI) algorithms play a crucial role in the analysis of gait data for early Parkinson’s diagnosis.
These algorithms can process large amounts of gait data and identify specific patterns that are indicative of Parkinson’s disease.
Machine learning techniques, a subset of AI, can be trained using gait data from both Parkinson’s patients and healthy individuals.
By comparing the data, the algorithm can learn to recognize the subtle differences in gait patterns and accurately identify individuals with Parkinson’s disease.
The use of AI in gait analysis not only improves the accuracy of Parkinson’s diagnosis but also allows for early detection.
As the algorithm becomes more refined with additional data, it has the potential to detect subtle changes in gait even before the clinical symptoms are noticeable.
The Benefits of Early Parkinson’s Diagnosis
Early diagnosis of Parkinson’s disease can significantly improve patient outcomes and facilitate better management of the condition. Some key benefits of early diagnosis include:.
1. Early Treatment: Early diagnosis allows for the prompt initiation of treatments and interventions that can alleviate symptoms and slow disease progression.
Medications, physical therapy, and lifestyle modifications can all play a role in improving the quality of life for individuals with Parkinson’s disease.
2. Enhanced Disease Management: With early diagnosis, healthcare professionals can closely monitor the progression of the disease and adjust treatment plans accordingly.
Regular assessments of gait and motor function can help in tracking the effectiveness of interventions and making timely adjustments to optimize outcomes.
3. Improved Quality of Life: Parkinson’s disease can significantly impact a person’s daily life, affecting their mobility, independence, and overall well-being.
Early diagnosis allows patients to take proactive steps to manage the condition, leading to improved physical function, reduced falls, and increased overall quality of life.
4. Research and Development: Early Parkinson’s diagnosis contributes to the advancement of scientific research and the development of new therapies.
By identifying individuals in the early stages of the disease, researchers can study the progression of Parkinson’s and test potential treatments more effectively.
Challenges and Limitations of Gait Analysis for Parkinson’s Diagnosis
While gait analysis holds promise for early Parkinson’s diagnosis, there are some challenges and limitations to consider.
1. Variability in Gait: Gait patterns can vary significantly among individuals, making it challenging to establish a definitive diagnostic threshold for Parkinson’s disease.
Normative data collected from a diverse population is essential to ensure accurate comparisons and avoid false positives or negatives.
2. Other Movement Disorders: Some movement disorders, such as essential tremor or atypical Parkinsonism, can exhibit similar gait abnormalities to Parkinson’s disease.
Gait analysis alone may not be sufficient to differentiate between these conditions, and additional clinical assessments may be needed for a comprehensive diagnosis.
3. Accessibility to Technology: Although wearable devices and smartphone applications offer convenient ways to collect gait data, not everyone has access to these technologies.
This can create disparities in early diagnosis and limit the use of gait analysis as a widespread screening tool.
The Future of Gait Analysis for Parkinson’s Diagnosis
Gait analysis has the potential to revolutionize the early diagnosis of Parkinson’s disease and improve patient outcomes.
Ongoing research and advancements in technology are likely to further enhance the accuracy and accessibility of gait analysis for Parkinson’s diagnosis.
Researchers are exploring the use of other sensors, such as pressure-sensitive insoles or smart shoes, to capture additional gait parameters and improve diagnostic accuracy.
Integration with wearable technology, such as smartwatches or fitness trackers, may also provide continuous monitoring of gait patterns, enabling early detection of subtle changes indicative of Parkinson’s disease.
Furthermore, collaborative efforts between researchers, clinicians, and technology developers are crucial to ensuring the development of reliable and user-friendly gait analysis tools.
Validation studies with large and diverse populations are essential to establish accurate diagnostic thresholds and minimize the risk of misdiagnosis.
Conclusion
Early Parkinson’s diagnosis is essential for optimal disease management and improved patient outcomes.
Gait analysis, through the use of wearable devices and AI algorithms, shows promise as a reliable and accessible method for early detection of Parkinson’s disease.
By analyzing an individual’s gait pattern, healthcare professionals can identify subtle changes indicative of Parkinson’s disease before clinical symptoms become evident.
Early diagnosis allows for timely interventions, better disease management, and enhanced quality of life for individuals living with Parkinson’s.